Anticholinergic Overload: Risks, Symptoms, and Safe Medication Use
When you take multiple medications that block acetylcholine, your body can hit a tipping point called anticholinergic overload, a dangerous buildup of effects from drugs that block the neurotransmitter acetylcholine, leading to confusion, dry mouth, urinary retention, and even delirium. Also known as anticholinergic burden, it’s not rare—it’s quietly affecting older adults and people on long-term meds for allergies, depression, or bladder issues. This isn’t just about one pill. It’s about the quiet accumulation of dozens of common prescriptions and even over-the-counter drugs that all do the same thing: shut down a key signal in your brain and nervous system.
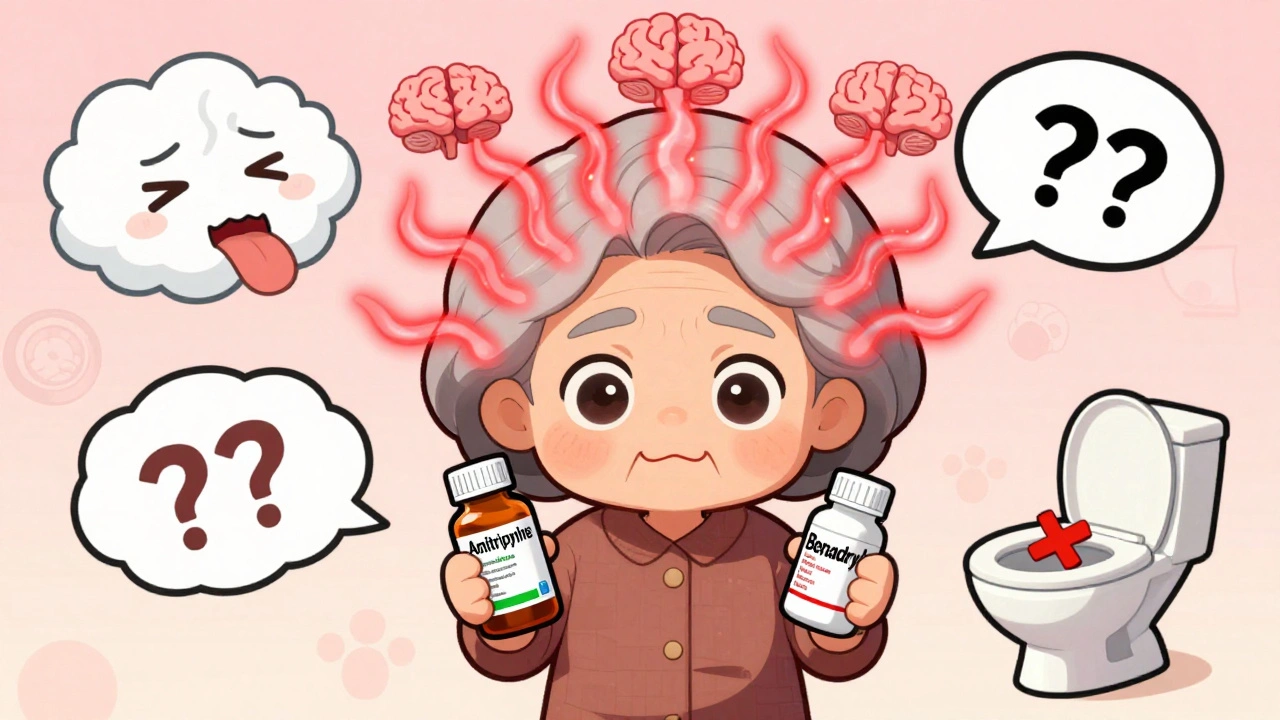
Think of your body’s acetylcholine like a dimmer switch for memory, muscle control, and digestion. When too many drugs turn that switch off, your brain can’t process information clearly, your bladder won’t empty, and your heart may race. Anticholinergic drugs, medications that inhibit acetylcholine activity, including many antihistamines, antidepressants, and bladder control pills are everywhere. Benadryl. Imipramine. Oxybutynin. Even some sleep aids and stomach meds. Combine them, and you’re stacking the odds. Older adults are especially vulnerable because their bodies clear these drugs slower, and their brains are more sensitive to the disruption. Studies show that taking three or more anticholinergic drugs at once raises the risk of dementia, falls, and hospitalization—no matter how well-intentioned the prescriptions are.
CNS depression, a slowdown of central nervous system activity caused by drug interactions, including anticholinergics combined with opioids or sedatives can sneak up on you. One day you’re fine. The next, you’re confused, dizzy, or unable to urinate. These aren’t just side effects—they’re warning signs of a system under strain. And it’s not just about age. People with Parkinson’s, epilepsy, or glaucoma are often prescribed anticholinergics without realizing how much they’re adding to the pile. The real danger? Most doctors don’t track it. Pharmacies don’t flag it. Patients don’t know to ask.
That’s why the posts below matter. They don’t just list drugs—they show you how to spot the hidden patterns. You’ll find real examples of how drug interactions, when two or more medications combine to produce unexpected or harmful effects push someone over the edge. You’ll see how a simple cold medicine mixed with a bladder pill can cause acute confusion in someone over 65. You’ll learn how to read labels for hidden anticholinergics, what questions to ask your pharmacist, and how to ask your doctor to review your whole list—not just one prescription at a time. This isn’t theoretical. These are stories of people who didn’t know they were at risk until it was too late. The fix isn’t always stopping meds. It’s knowing which ones to swap, reduce, or replace before the overload hits.