Anticholinergic Burden Calculator
This tool calculates your Anticholinergic Cognitive Burden (ACB) score based on medications you're taking. A score of 3 or higher doubles dementia risk over three years. This information helps identify potential risks from combining drugs like tricyclic antidepressants and antihistamines.
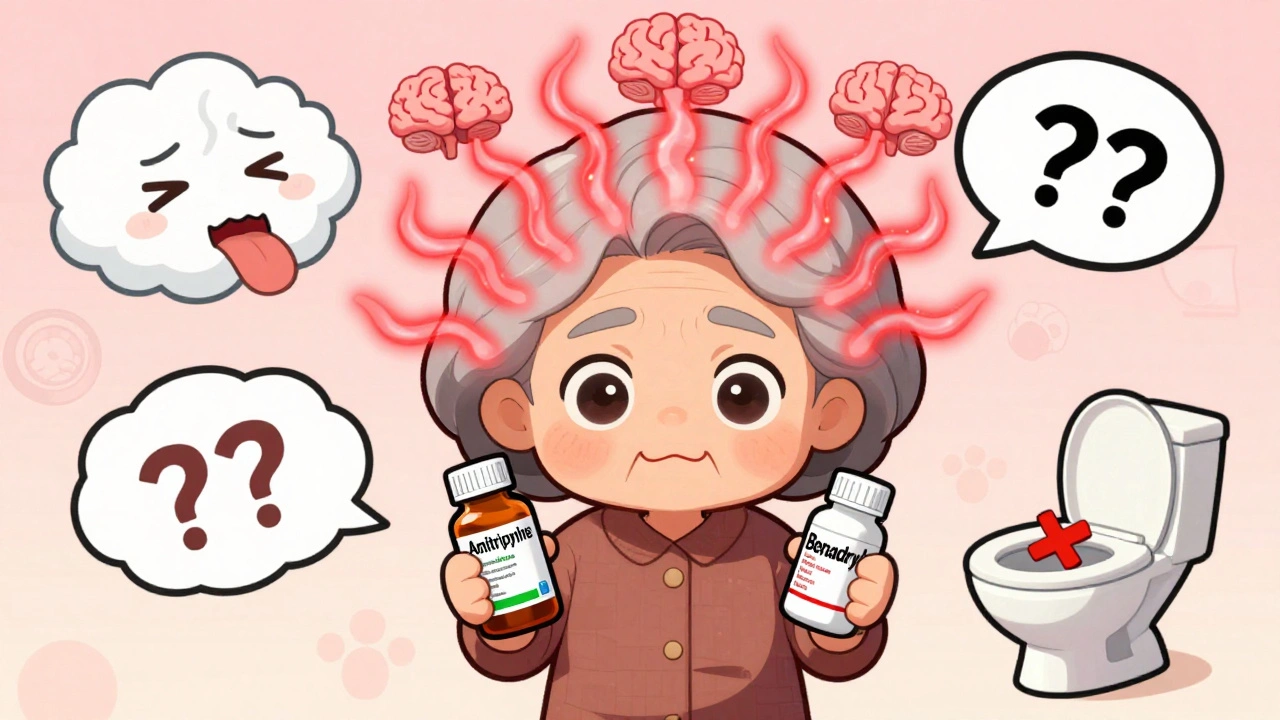
Many people take tricyclic antidepressants (TCAs) for chronic pain, depression, or anxiety. Others reach for over-the-counter antihistamines like diphenhydramine (Benadryl) for allergies, colds, or trouble sleeping. What most don’t realize is that combining these two types of drugs can push the body into a dangerous state called anticholinergic overload. It’s not rare. It’s not theoretical. It’s happening in clinics and emergency rooms right now-especially in older adults.
What Is Anticholinergic Overload?
Your body uses acetylcholine, a key neurotransmitter, to control everything from memory and attention to digestion, heart rate, and bladder function. Anticholinergic drugs block this chemical. One drug might cause mild dry mouth or drowsiness. But when you stack two or more drugs that do the same thing, the effects add up. That’s anticholinergic overload.Tricyclic antidepressants like amitriptyline (Elavil), imipramine (Tofranil), and clomipramine (Anafranil) were developed in the 1950s. They work by boosting serotonin and norepinephrine-but they also strongly block muscarinic acetylcholine receptors. First-generation antihistamines like diphenhydramine and hydroxyzine were designed to fight allergies by blocking histamine. But they also block acetylcholine receptors with nearly the same strength. When taken together, their effects aren’t just added-they’re multiplied.
Who’s at Risk?
Older adults are most vulnerable. As we age, our liver and kidneys slow down. Drugs stay in the system longer. The brain becomes more sensitive to acetylcholine loss. A 2022 study found that people over 65 who took both a TCA and diphenhydramine had a 200% higher risk of sudden confusion or delirium-even after just 30 days of use.It’s not just seniors. Anyone taking multiple medications is at risk. A 2020 study of over 3,300 patients showed that 6,814 high-risk drug interaction alerts were triggered by TCA-antihistamine combinations. One patient in the study was prescribed fluoxetine, sertraline, amitriptyline, tramadol, lorazepam, and alprazolam-all at once. That’s six CNS depressants, many with anticholinergic properties. It’s a recipe for disaster.
What Happens When Overload Occurs?
The symptoms don’t always look like a drug reaction. They look like aging, dementia, or depression getting worse:- Severe confusion or disorientation
- Memory lapses that come on suddenly
- Difficulty speaking or finding words
- Blurred vision
- Urinary retention (can’t pee)
- Constipation so bad it requires hospitalization
- Fast heartbeat, dry mouth, flushed skin
- Hallucinations or delusions
One user on Psych Forums described ending up in the ER after adding Benadryl to amitriptyline: “I couldn’t remember my own name for hours. They said I had anticholinergic toxicity.” Another Reddit user, a medical resident, said they’d seen at least three elderly patients admitted with delirium traced directly to this combo.

Why Do Doctors Still Prescribe This?
It’s not always negligence. Many doctors don’t realize how common this interaction is. TCAs are still first-line for neuropathic pain, fibromyalgia, and some types of depression. Diphenhydramine is cheap, available without a prescription, and often used as a sleep aid. Patients don’t always tell their doctors they’re taking OTC meds. And until recently, electronic health records didn’t flag these combinations strongly.That’s changing. Since 2022, major EHR systems like Epic now trigger hard stops when a prescriber tries to write both a TCA and diphenhydramine together. Alerts are shown in 92% of attempted co-prescriptions. Still, many slips through-especially in primary care settings where time is tight.
How to Measure the Risk: The ACB Scale
Clinicians now use the Anticholinergic Cognitive Burden (ACB) scale to rate how strong a drug’s anticholinergic effect is:- Amitriptyline = Score 3 (highest risk)
- Diphenhydramine = Score 2
- Loratadine (Claritin) = Score 0
- Desipramine = Score 1
When you add two drugs with scores of 3 and 2, you get a total of 5. Research shows that a cumulative ACB score of 3 or higher doubles the risk of dementia over three years. A score of 5? That’s a red flag. The American Geriatrics Society’s Beers Criteria (2023) explicitly says: “Avoid first-generation antihistamines in older adults taking TCAs.”
What Are the Safer Alternatives?
You don’t have to give up sleep or allergy relief. There are better options:- Switch antihistamines: Use loratadine (Claritin), fexofenadine (Allegra), or cetirizine (Zyrtec). These second-generation antihistamines have almost no anticholinergic activity. They’re just as effective for allergies and cause far less drowsiness.
- For sleep: Try melatonin (0.5-5 mg). It’s not addictive, doesn’t block acetylcholine, and works well for circadian rhythm issues. Avoid doxylamine (Unisom) too-it’s just another strong anticholinergic.
- For pain or depression: If you’re on amitriptyline and having side effects, ask about switching to nortriptyline or desipramine. They’re still TCAs, but with lower anticholinergic burden. Or consider an SSRI like sertraline or escitalopram, which have less than 10% of the anticholinergic risk.

The Long-Term Danger: Dementia Risk
This isn’t just about confusion in the hospital. It’s about your brain over time. A landmark 2015 study in JAMA Internal Medicine followed over 3,400 people for more than 10 years. Those who took high-anticholinergic medications for three years or more had a 54% higher risk of developing dementia. The risk climbed with each additional anticholinergic drug. That’s not a small number. It’s a public health issue.A 2023 study in the Journal of the American Geriatrics Society showed that when doctors helped patients stop these drugs, their cognitive function improved by 34% in just 18 months. That’s not just stabilization. That’s recovery.
What You Should Do Right Now
If you’re taking a TCA like amitriptyline, imipramine, or clomipramine:- Check your medicine cabinet. Do you have diphenhydramine, hydroxyzine, doxylamine, or promethazine? Stop taking them unless your doctor says otherwise.
- Ask your doctor or pharmacist to run your full list of medications through an ACB calculator. Many pharmacies now have free tools for this.
- If you’re using an OTC sleep aid, switch to melatonin. It’s safer, non-habit forming, and doesn’t mess with your brain chemistry.
- Don’t assume your doctor knows you’re taking something OTC. Always tell them-even if you think it’s “just Benadryl.”
And if you’re caring for an older parent or relative: watch for sudden changes in behavior. Confusion, memory loss, or trouble urinating after starting a new medication? That’s not normal aging. That’s a medical emergency.
The Bigger Picture
Prescriptions for TCAs have dropped from 25% of antidepressant use in 1990 to just 5% today. That’s progress. But they’re still used for pain, and many patients are stuck on them. Meanwhile, over-the-counter antihistamines are more popular than ever. The FDA now requires updated warnings on both drug classes. The National Institute on Aging is funding a $2.4 million study to track long-term cognitive damage from these combinations.What’s clear is this: anticholinergic overload isn’t a side effect. It’s a preventable iatrogenic illness-one that’s been hiding in plain sight for decades. We’ve known about it since the 1980s. We’ve measured it. We’ve named it. Now we just need to stop letting it happen.
Can I take Benadryl with amitriptyline?
No. Combining diphenhydramine (Benadryl) with amitriptyline significantly increases the risk of anticholinergic overload. Both drugs block acetylcholine, and together they can cause confusion, urinary retention, rapid heartbeat, and even delirium. This combination is flagged as high-risk by the American Geriatrics Society and major EHR systems. Switch to a non-anticholinergic sleep aid like melatonin instead.
Are all antihistamines dangerous with TCAs?
No. Only first-generation antihistamines like diphenhydramine, hydroxyzine, and promethazine have strong anticholinergic effects. Second-generation antihistamines like loratadine (Claritin), fexofenadine (Allegra), and cetirizine (Zyrtec) have minimal to no anticholinergic activity. They’re safe to use with TCAs and are the preferred choice for allergy relief.
Do all tricyclic antidepressants have the same risk?
No. Amitriptyline and clomipramine have the highest anticholinergic burden (ACB score of 3). Nortriptyline and desipramine are TCAs too, but they’re weaker at blocking acetylcholine (ACB score of 1). If you’re on a TCA and experiencing side effects, ask your doctor if switching to one of these lower-risk options is possible.
Can anticholinergic overload cause permanent damage?
Long-term exposure increases dementia risk by 54%, according to JAMA Internal Medicine. But the good news is that stopping these drugs can lead to cognitive improvement. A 2023 study showed a 34% improvement in cognitive function within 18 months after deprescribing anticholinergics. The damage isn’t always permanent-if caught early.
How do I know if I’m experiencing anticholinergic overload?
Watch for sudden changes: confusion, memory loss, trouble urinating, dry mouth, blurred vision, constipation, or a racing heart. If you’ve recently started or increased a TCA or antihistamine and notice these symptoms, stop the OTC drug immediately and contact your doctor. Don’t wait. This can be life-threatening.
If you’re on a TCA and taking any OTC sleep or allergy medicine, don’t wait for a crisis. Review your meds today. Talk to your pharmacist. Ask for alternatives. Your brain will thank you.



so like... i took benadryl for my allergies last week and also my amitriptyline for back pain?? and then i spent 3 hours staring at the wall wondering why my cat was speaking in latin?? turns out i'm a walking clinical trial. thanks for the wake up call, i guess??
This is not merely a pharmacological concern-it is a systemic failure of medical education, regulatory oversight, and patient advocacy. The continued prevalence of this interaction reflects a profound institutional negligence that endangers public health. I urge all clinicians to implement mandatory ACB scoring prior to prescribing any anticholinergic agent.
I’m so glad this is getting more attention. I’ve seen elderly patients in my clinic confuse their own grandchildren for strangers after starting Benadryl with a TCA. It’s heartbreaking-and entirely preventable. Please, if you’re on one of these meds, talk to your pharmacist. They’re the unsung heroes of medication safety.
Let me be perfectly clear: America is drowning in lazy medicine. Doctors prescribe TCAs like they’re candy, and patients pop Benadryl like it’s a vitamin-because they’re told it’s ‘harmless.’ But here’s the truth: Your brain isn’t a machine you can overload without consequences. We’ve known this since the 1980s-and yet, here we are. This isn’t ‘side effects’-this is cultural negligence. And I’m tired of it.
I appreciate how thorough this is. I’ve been on nortriptyline for years and used Zyrtec for allergies-never realized how much safer that combo was. It’s easy to feel overwhelmed by meds, but knowing there are alternatives makes it feel less scary. Thanks for breaking it down without fear-mongering.
I find it deeply troubling that people treat their own health with such casual disregard. If you cannot be responsible enough to read a label or consult a professional before combining medications, then perhaps you should not be allowed to self-medicate at all. This is not a matter of personal freedom-it is a matter of public safety.
lol y’all act like this is news. i’ve been telling my grandma for years not to take benadryl with her elavil. she says ‘but it helps me sleep!’ yeah, because it turns your brain into a soggy cereal box. also-claritin is not ‘just as good’-it’s 10x better. and if you think melatonin is a ‘sleep aid,’ you’re doing it wrong. it’s a circadian signal, not a sedative. grow up.
In India, we have long understood the dangers of polypharmacy. Our elders rarely take OTC antihistamines precisely because they respect the body’s chemistry. Western medicine has become a carnival of pills-each one promising relief, but none offering wisdom. This is not a drug interaction-it is a spiritual failure. We treat symptoms, not systems. We must return to balance.
I was on amitriptyline for fibro and started taking hydroxyzine for anxiety-ended up in the ER with urinary retention and hallucinations. They said I had ‘acute anticholinergic syndrome.’ I didn’t even know that was a thing. Now I take sertraline and loratadine. My brain feels like it’s been unplugged from a static charger. Don’t wait for a crisis.