What Pharmacists Really Think About Switching to Generic Drugs
Every day, pharmacists face a quiet but persistent challenge: patients walk in with a prescription for a brand-name drug, and the system automatically suggests a cheaper generic version. It’s supposed to be simple-same active ingredient, same effect, lower price. But in practice, it’s anything but straightforward. Pharmacists aren’t just filling prescriptions. They’re managing expectations, fighting misconceptions, and sometimes playing mediator between patients, doctors, and insurance companies-all in a five-minute window between other customers.
The FDA says generics are just as safe and effective as brand-name drugs. They require bioequivalence within 80-125% of the original, and over 2,000 studies back that up. The average difference in how the body absorbs the drug? Just 3.5%. That’s less than the natural variation you’d see if the same person took the same pill twice on different days. Yet, despite the science, many patients still don’t believe it.
Patients Don’t Trust the Generic
It’s not about the drug. It’s about the pill.
Patients recognize their medication by how it looks-color, shape, size, even the imprint on the tablet. When they get a different-looking pill, even if it’s the exact same medicine, they think something’s wrong. One woman in Seattle told her pharmacist she stopped taking her blood pressure pill because it was “too small and white now.” She didn’t realize the brand had changed manufacturers. Her blood pressure spiked two weeks later.
That’s not rare. Studies show about one-third of patients report negative experiences after switching to generics. Some blame the pill for side effects that never happened before. Others think the lower price means lower quality. “If it’s so good, why is it so cheap?” is a question pharmacists hear daily. And they can’t just shrug it off. A patient who doubts their medication is more likely to skip doses, stop taking it altogether, or end up back in the ER.
Older patients, especially those on multiple medications, are most vulnerable. One pharmacist in Portland described a man with dementia who kept asking why his “blue pill” was now yellow. He refused to take it until his daughter called the doctor. That’s 20 minutes of the pharmacist’s day lost-not because the drug was unsafe, but because the patient didn’t trust the change.
The Doctors Aren’t Helping
Here’s the kicker: most patients have no idea substitution even happens.
A national survey found that 64% of patients never heard from their doctor that a generic version was available. That means pharmacists are the first-and often only-source of information. And they’re expected to explain it all during a rushed counseling session, usually while someone else is waiting at the pickup window.
Worse, many physicians don’t know the rules themselves. Some still believe generics are “inferior” for certain drugs, especially those with narrow therapeutic indexes-like warfarin, levothyroxine, or anti-seizure medications. Even though the FDA approves these generics, some doctors automatically write “dispense as written” on the prescription, not because of clinical risk, but because they’re unsure.
Pharmacists are caught in the middle. They know the science. They know the guidelines from ASHP and the FDA. But if a doctor says “no substitutions,” they can’t override it-even if the patient is paying $200 a month for a drug that has a $15 generic equivalent. That’s not just expensive. It’s unfair.

The Hidden Burden: Time and Education
Teaching a patient about generic substitution isn’t a one-sentence explanation. It’s a conversation.
“This is the same medicine, just made by a different company,” sounds simple. But patients need context. They need to know why the pill looks different. Why the name on the bottle changed. Why their insurance pushed this switch. And they need to feel heard.
One study found that only 38% of patients were told they could refuse the generic. That’s not informed consent-that’s a missed opportunity. And when patients are confused, they often demand to speak with their doctor. That means pharmacists have to call or fax the office, wait on hold, and then explain the situation again. One pharmacist in Chicago estimated that 20% of her day was spent managing substitution-related calls and paperwork.
And it’s worse for patients on complex regimens. Someone taking five medications, each with a different generic version, can end up with a pill organizer that looks like a rainbow. No wonder adherence drops. Pharmacists know this. But they’re not trained counselors. They’re not given extra time. And they’re not paid extra to do this emotional labor.
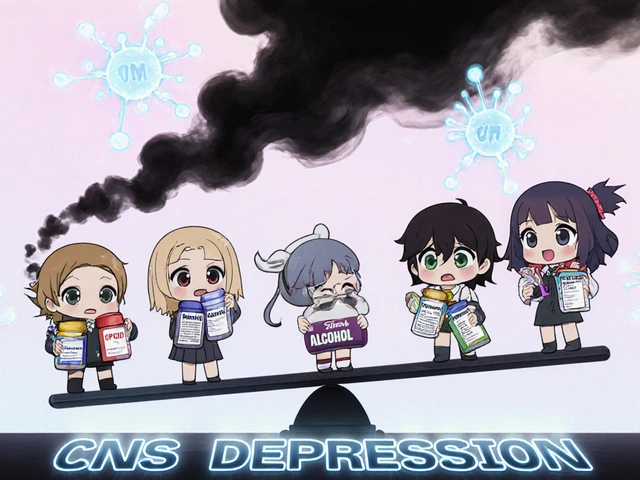
Where Substitution Gets Risky
Not all drugs are created equal when it comes to substitution.
For most medications-antibiotics, statins, antidepressants-the switch is seamless. But for drugs with a narrow therapeutic index (NTI), even small changes in absorption can matter. Levothyroxine, for example, is used to treat hypothyroidism. A tiny shift in how much the body absorbs can throw off hormone levels, leading to fatigue, weight gain, or heart problems. The FDA says generics for these drugs are safe. But pharmacists still tread carefully. Many will only substitute if the patient has been stable on the same generic for months. Others avoid it entirely unless the prescriber specifically allows it.
Biosimilars add another layer. These aren’t your typical generics. They’re complex biologic drugs-like insulin or rheumatoid arthritis treatments-that can’t be copied exactly. They’re similar, but not identical. The FDA requires extra testing, and pharmacists need to know when substitution is allowed. Some states require prescriber approval. Others let pharmacists switch automatically. The rules vary. The confusion doesn’t.

What Works: Real Solutions from the Front Lines
Some pharmacies have found ways to make this work.
One clinic in Minnesota started handing out simple, one-page handouts with pictures of the brand and generic versions side by side. They included the active ingredient, why the pill looks different, and a note: “This is approved by the FDA as equally effective.” Patient questions dropped by 40% in six months.
Another pharmacy in Ohio began training staff to ask one question at pickup: “Have you taken this medicine before?” If the answer is no, they pause and explain the substitution. If it’s yes, they ask, “Did you notice the pill looks different?” That opens the door to a real conversation instead of a rushed warning.
And some pharmacists are pushing for change. They’re asking doctors to mention generics during visits-not as an afterthought, but as a normal part of treatment. “We’re not just saving you money,” one pharmacist told a group of local physicians. “We’re helping you keep your patients on their meds.”
It’s Not Just About Cost
Generic substitution was designed to cut costs. And it has-patients save an average of 21% on prescriptions. But the real win isn’t the price tag. It’s the adherence.
When patients understand what they’re taking and trust it, they take it. When they don’t, they stop. And that’s when health problems start. Pharmacists aren’t trying to force a cheaper pill on anyone. They’re trying to make sure the right medicine stays in the patient’s hand-and in their body.
The system is broken, not because generics don’t work, but because we treat them like a cost-cutting trick instead of a medical tool. Until doctors, insurers, and patients start seeing generics the way pharmacists do-as safe, effective, and essential-this tension won’t go away.
And until then, pharmacists will keep answering the same questions, explaining the same science, and quietly holding the line between cost and care.
Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also be bioequivalent, meaning they’re absorbed into the body at the same rate and to the same extent-within a 3.5% average difference, which is less than natural variation in how your body processes the same drug on different days. Over 2,000 studies confirm this. For most medications, there’s no clinical difference.
Why do generic pills look different from brand-name ones?
The appearance-color, shape, size-is determined by the manufacturer and can’t be copied exactly due to trademark laws. But the active ingredient, dose, and how it works in your body are identical. The different look doesn’t mean it’s weaker or less effective. It just means a different company made it.
Can pharmacists substitute any generic drug?
No. State laws and prescriber instructions control substitution. Some drugs, especially those with a narrow therapeutic index-like warfarin, levothyroxine, or anti-seizure medications-require extra caution. Some doctors write “dispense as written” on the prescription, meaning substitution isn’t allowed. Pharmacists must follow those instructions, even if a cheaper generic is available.
Can I refuse a generic substitution?
Yes. You have the right to refuse a generic substitution and ask for the brand-name drug instead. However, your insurance may not cover the full cost, and you’ll likely pay more out of pocket. Pharmacists should always inform you of this option, but in practice, many don’t. If you’re unsure, ask: “Can I get the brand version instead?”
Why do some pharmacists hesitate to substitute for certain medications?
For drugs with a narrow therapeutic index, even small changes in how the body absorbs the drug can affect treatment. While generics for these drugs are approved by the FDA, pharmacists often prefer to keep patients on the same version they’ve been stable on-whether brand or generic-to avoid any risk of instability. It’s not about distrust in generics-it’s about minimizing risk for patients who are already vulnerable.
Do biosimilars work the same way as regular generics?
No. Biosimilars are not exact copies like traditional generics. They’re complex biologic drugs made from living cells, so they can’t be replicated perfectly. They’re highly similar, but not identical. The FDA requires extra testing to prove they work the same way. Substitution rules for biosimilars are stricter and vary by state. Some require prescriber approval, and pharmacists must be trained to handle them differently than small-molecule generics.
Why don’t doctors talk to patients about generics?
Many doctors don’t have time during appointments, or they assume the pharmacist will handle it. Others still believe generics are inferior for certain conditions, even though evidence doesn’t support that. Studies show patients are more likely to accept generics when their doctor mentions them upfront. But too often, the conversation never happens-leaving pharmacists to fill the gap.
How can I tell if my medication has been switched to a generic?
Check the label. The generic manufacturer’s name will appear instead of the brand name. The pill may look different in color, shape, or size. You can also ask your pharmacist: “Is this the brand or generic version?” They’re required to answer. If you notice changes in how you feel after switching, tell your pharmacist or doctor-don’t assume it’s your fault.