When it comes to losing weight with medication, you’re not just choosing between pills and shots-you’re choosing between two entirely different approaches to how your body handles hunger, fat, and metabolism. On one side, there are the older weight loss drugs that have been around for decades. On the other, there’s the new wave of GLP-1 agonists like Wegovy, Zepbound, and Saxenda-medications that have reshaped the entire weight loss landscape in just a few years.
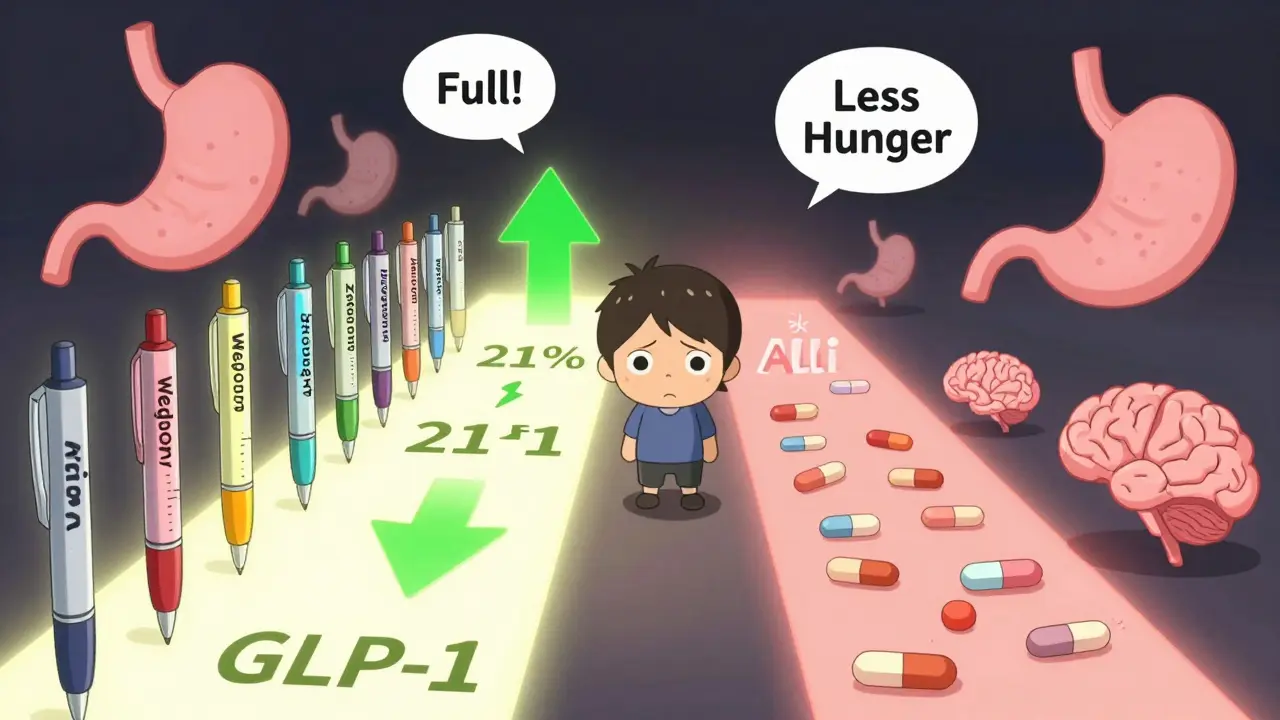
How GLP-1 Agonists Actually Work
GLP-1 agonists aren’t just appetite suppressants. They mimic a natural hormone your body already makes called glucagon-like peptide-1. This hormone tells your brain you’re full, slows down how fast your stomach empties, and helps your pancreas release insulin when you eat. In simple terms: you feel full sooner, stay full longer, and your body handles sugar better.
Drugs like semaglutide (Wegovy), tirzepatide (Zepbound), and liraglutide (Saxenda) are injected once a week or once a day. They don’t burn fat directly. Instead, they rewire your hunger signals. In clinical trials, people using Wegovy lost an average of 15% of their body weight. Zepbound, which also targets a second hormone (GIP), pushed that number to nearly 21% in some studies. That’s not just a few pounds-it’s often 30 to 50 pounds lost over a year.
These medications were originally designed for type 2 diabetes. But their weight loss effects were so strong that the FDA approved them specifically for obesity. Today, they’re the most prescribed weight loss drugs in the U.S., taking over 78% of new prescriptions in early 2024.
What the Older Drugs Do-and Don’t Do
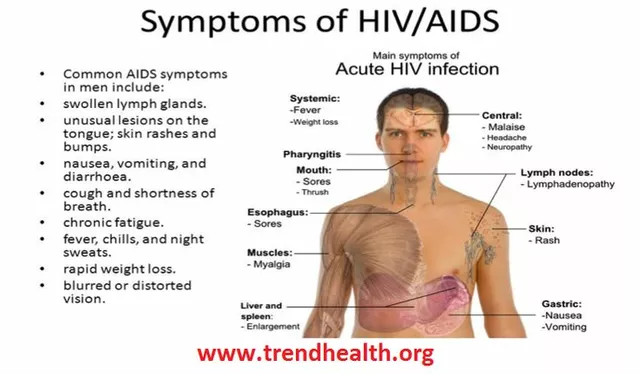
Before GLP-1 agonists, the main options were pills like orlistat (Alli, Xenical), phentermine-topiramate (Qsymia), and naltrexone-bupropion (Contrave). These work differently-and less powerfully.
Orlistat blocks fat absorption in your gut. About 30% of the fat you eat just passes through your body. That sounds good until you realize it leads to oily stools, frequent bathroom trips, and the need to take it with every meal. It typically results in 5-10% weight loss.
Qsymia combines a stimulant (phentermine) with an anti-seizure drug (topiramate) to reduce appetite. It works for some, but side effects include dry mouth, tingling in hands and feet, and increased heart rate. It averages about 10% weight loss.
Contrave uses naltrexone (used for addiction) and bupropion (an antidepressant) to target the brain’s reward system. It helps curb cravings, especially for sugary or fatty foods. But it doesn’t stop hunger-it just makes food feel less appealing. Weight loss averages 5-8%.
None of these come close to the 15-20% range of GLP-1 drugs. Even Saxenda, which is itself a GLP-1 agonist, only hits about 8% on average-because it’s a lower dose than Wegovy.
The Real-World Gap Between Trials and Reality
It’s easy to get excited by clinical trial numbers. But what happens when real people start taking these drugs?
A 2024 study from NYU Langone Health tracked over 50,000 people using GLP-1 medications for weight loss. After six months, the average weight loss was only 4.7%. After a full year, it was 7%. That’s less than half of what the trials promised.
Why? Because most people don’t stay on the medication. About 70% stop within a year. Why? Two big reasons: side effects and cost.
Nausea, vomiting, and stomach pain are common during the first few months-especially when the dose is being increased. One in five people quit because they couldn’t tolerate the GI issues. Others couldn’t afford it.

Cost: The Hidden Barrier
Wegovy and Zepbound cost between $1,000 and $1,400 a month without insurance. That’s more than most people pay for rent or car payments. Even with coupons, annual savings are capped at $500-$1,000-barely making a dent.
Compare that to phentermine, which can cost $10-$50 a month. Orlistat runs $30-$80. Even Qsymia and Contrave are usually under $150 a month with insurance.
Insurance coverage is a nightmare. Only 28% of commercial plans cover GLP-1 drugs for weight loss without strict requirements. Many require a BMI over 35 with a related condition like high blood pressure or diabetes. Some won’t cover them at all unless you’ve tried and failed diet and exercise first.
For many, the cost isn’t just high-it’s impossible.
Side Effects: More Than Just Nausea
Yes, nausea is common. But it’s not the only problem.
Some users report severe stomach issues-delayed gastric emptying, gastroparesis-like symptoms, chronic bloating. A growing number on Reddit and patient forums describe months of discomfort, even after reaching their target dose.
There’s also the risk of rebound weight gain. Studies show that if you stop taking a GLP-1 agonist, you’ll likely regain most-if not all-of the weight you lost. One study in JAMA Surgery found that 50-100% of people regained weight within a year of stopping.
And while these drugs are safe for most, they’re not risk-free. They carry a boxed warning for thyroid tumors in rodents. It’s unclear if that applies to humans, but it’s something your doctor should discuss with you.
Who Benefits the Most?
GLP-1 agonists aren’t for everyone. But they’re a game-changer for certain people:
- Those with obesity (BMI ≥30) who’ve tried diet and exercise without lasting results
- People with type 2 diabetes who need better blood sugar control AND weight loss
- Those willing to commit to weekly injections and tolerate side effects
- People with insurance that covers the drug-or who can afford it out-of-pocket
For others, older drugs might still make sense. If you can’t handle injections, can’t afford the cost, or have a history of anxiety or heart issues, Qsymia or Contrave might be safer options. Orlistat could work if you’re okay with digestive side effects and just need a gentle nudge.

Surgery vs. Pills: The Long-Term View
When you look at long-term results, surgery still wins.
The same NYU study found that people who had bariatric surgery lost 24% of their body weight after two years. That’s more than double what most GLP-1 users achieve in a year. And the weight loss tends to stick.
That’s why experts like the American Society for Metabolic and Bariatric Surgery say surgery should still be considered the gold standard for severe obesity. But surgery isn’t for everyone. It’s invasive, requires lifelong dietary changes, and isn’t covered by all plans.
Many people now use GLP-1 drugs as a bridge-losing weight before surgery to reduce surgical risk. Others use them after surgery to maintain results if weight starts creeping back.
What’s Next? The Future of Weight Loss Drugs
The next wave is already here. Retatrutide, a triple agonist that targets GLP-1, GIP, and glucagon, showed up to 24.2% weight loss in early trials. MariTide, a new monoclonal antibody, is in Phase 3 testing and could offer similar results without injections.
By 2027, analysts predict GLP-1 drugs will make up 85% of the weight loss market. But if prices don’t drop and coverage doesn’t improve, they’ll remain out of reach for most Americans.
For now, the choice isn’t just about which drug is stronger-it’s about what you can live with, afford, and stick to.
Practical Tips If You’re Considering One
- Start low, go slow. Most side effects happen during dose escalation. Your doctor should increase your dose gradually over 4-5 months.
- Use anti-nausea meds like ondansetron temporarily if needed. Many patients find relief.
- Work with a specialty pharmacy-they handle prior authorizations better than regular pharmacies.
- Check manufacturer assistance programs. Novo Nordisk (Wegovy) and Eli Lilly (Zepbound) offer coupons and patient support.
- Track your progress. Weight loss isn’t linear. Some weeks you’ll lose more, some weeks you’ll plateau. That’s normal.
- Don’t expect miracles. These drugs work best with diet and movement. They’re tools, not magic.
There’s no single best drug. The best one is the one you can take consistently-and afford.