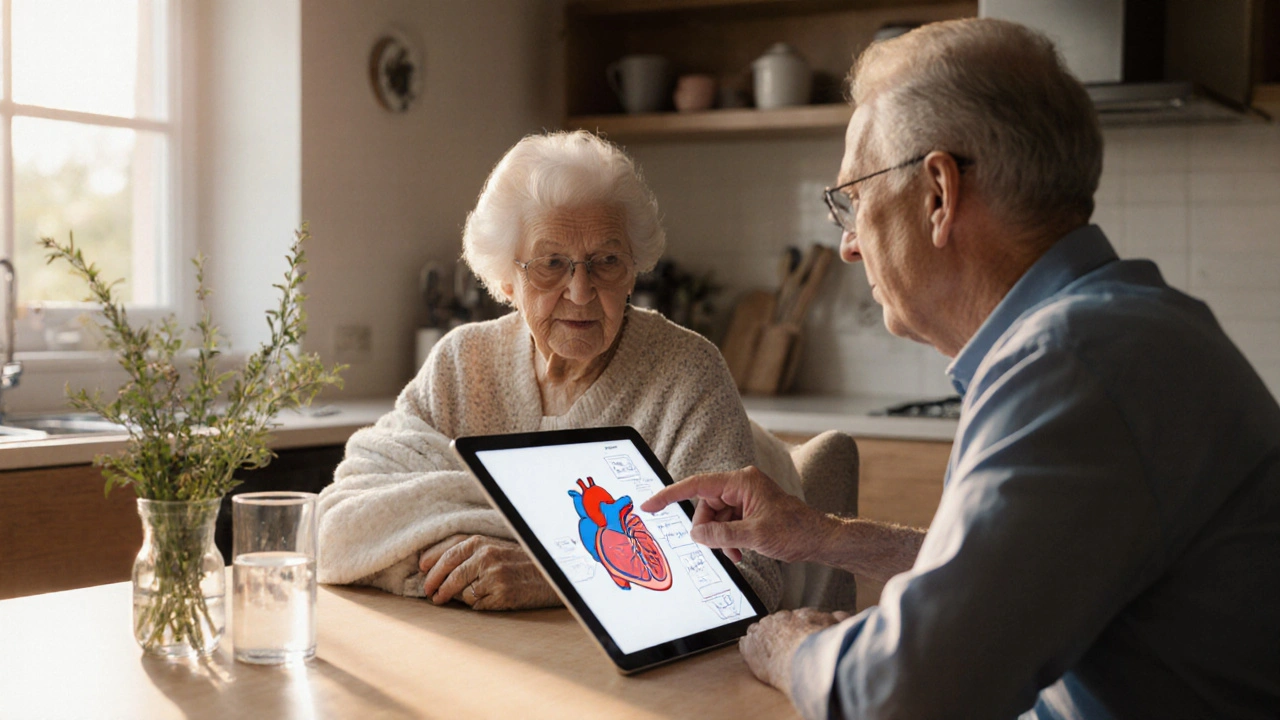
Elderly Heart Failure Care: What You Need to Know
When working with Elderly Heart Failure Care, a coordinated strategy for handling chronic heart failure in older adults. Also known as senior cardiac management, it aims to keep symptoms low, preserve quality of life, and prevent costly hospital trips.
At its core, heart failure, a condition where the heart cannot pump enough blood to meet the body’s needs becomes more challenging as patients age. Age‑related changes like reduced kidney function, frailty, and multiple co‑existing illnesses mean the treatment plan must be flexible. The elderly patient, any individual typically over 65 dealing with chronic health issues often requires lower drug doses, careful monitoring for side effects, and extra support for daily tasks.
Key Pillars of Effective Care
Medication management is the backbone of elderly heart failure care. Classic agents such as digoxin, a cardiac glycoside that improves heart contractility and slows down the heart rate still have a role, especially when patients cannot tolerate newer drugs. Yet digoxin’s narrow therapeutic window demands regular blood‑level checks, a routine often coordinated with primary‑care physicians.
Equally important are diuretics, medications that help the body eliminate excess fluid, reducing the workload on the heart. Loop diuretics like furosemide are frequently prescribed, but seniors may need potassium‑sparing options to avoid dangerous electrolyte shifts. Pairing diuretics with a blood pressure medication, drugs such as ACE inhibitors, ARBs, or calcium‑channel blockers that lower systemic pressure creates a synergistic effect: the heart pumps more efficiently while the vessels stay relaxed.
Beyond pills, lifestyle tweaks make a measurable difference. Fluid restriction, usually to about 1.5‑2 L per day, helps prevent sudden weight gain from water retention. Sodium intake should stay below 2 g daily, and regular, low‑impact exercise—like walking or seated cycling—keeps muscles strong without overtaxing the heart. Monitoring tools, including home blood‑pressure cuffs and weight scales, let seniors and caregivers spot early warning signs such as a 2‑kg rise in weight over three days.
Education and support round out the care model. Patients who understand why they take each medication, how to recognize side‑effects, and when to call a doctor are more likely to stick to their regimen. Caregiver involvement, medication reviews every three months, and coordinated communication between cardiologists, GPs, and pharmacists reduce the risk of prescription conflicts, especially when polypharmacy is a concern.
All these elements—precise drug choices, fluid and sodium control, regular monitoring, and clear education—interact to form a robust plan. The next section of this page lists articles that dive deeper into each component, from the science behind digoxin to practical tips for managing blood pressure meds in seniors.
Ready to explore specific drug comparisons, dietary strategies, and symptom‑tracking tools? Below you’ll find a curated collection that breaks down each piece of the puzzle, giving you actionable insight for better elderly heart failure care.