Elderly Heart Failure Medication Calculator
Medication Dosing Calculator
Results will appear here after calculating.
When heart failure in the elderly presents unique challenges, clinicians must blend evidence‑based heart failure therapy with age‑specific considerations, the goal shifts from merely prolonging life to preserving quality and independence.
Understanding Heart Failure in Older Adults
Heart failure is a condition where the cardiovascular system fails to pump enough blood to meet the body’s needs. In people over 65, structural changes like arterial stiffening, reduced myocardial compliance, and impaired autonomic regulation make the heart less resilient to stress. Consequently, symptoms such as dyspnea, fatigue, and peripheral edema appear earlier and progress faster than in younger patients.
Key Clinical Features and Diagnostic Nuances
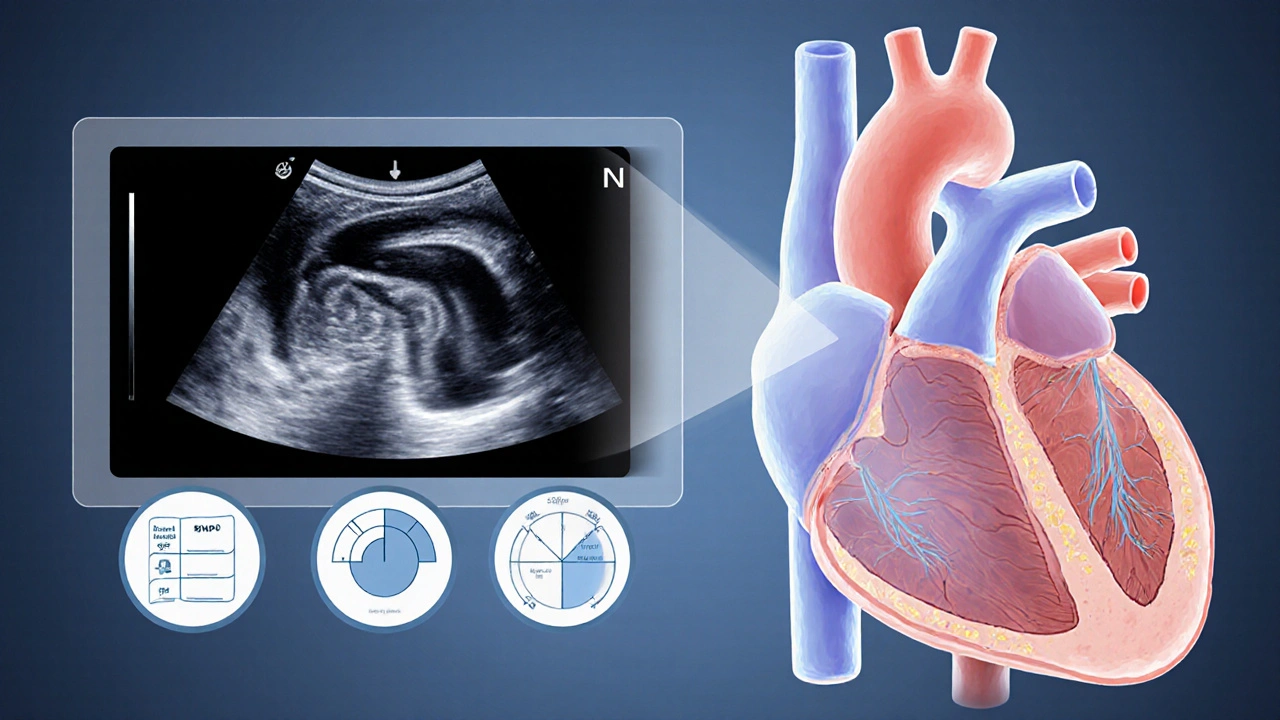
Accurate diagnosis hinges on both history and objective measures. The ejection fraction (EF) quantifies the percentage of blood expelled from the left ventricle with each beat remains the cornerstone metric. An EF below 40% typically signals systolic dysfunction, while a preserved EF (≥50%) points to diastolic dysfunction, which dominates in the elderly.
Blood tests for B‑type natriuretic peptide (BNP) rise when the heart is under pressure and fluid overload is present help differentiate cardiac from pulmonary causes of breathlessness. Imaging, especially echocardiography, must be interpreted with age‑adjusted normal ranges; for instance, a mild increase in left‑ventricular wall thickness is common after 70 years and does not always equate to pathology.
Tailored Pharmacologic Strategies
Standard heart‑failure drugs - ACE inhibitors, beta‑blockers, mineralocorticoid receptor antagonists, and loop diuretics - remain effective, but dosing needs careful titration.
- ACE inhibitor reduces afterload and slows ventricular remodeling: Start at half the typical adult dose; monitor renal function and potassium weekly for the first month.
- beta‑blocker blunts sympathetic overdrive, improving survival: Use carvedilol or bisoprolol at low doses (1.25mg once daily) and increase slowly; watch for bradycardia and orthostatic drops.
- diuretic therapy relieves congestion by promoting fluid excretion: Loop diuretics such as furosemide are first‑line, but start at 20mg oral once daily, adjusting based on weight loss and electrolyte trends.
- mineralocorticoid receptor antagonist offers mortality benefit but raises hyperkalemia risk: Consider spironolactone only if potassium stays below 5.0mmol/L and eGFR >30mL/min/1.73m².
Older adults often require dose reductions because of decreased hepatic clearance and increased sensitivity to drug‑induced hypotension. The mantra is “start low, go slow, and monitor closely.”
Managing Frailty and Polypharmacy
Frailty describes a state of reduced physiological reserve and heightened vulnerability to stressors is common in heart‑failure patients over 80. A simple Fried Frailty Phenotype assessment (weight loss, exhaustion, grip strength, walking speed, activity) helps stratify risk. Those identified as frail benefit from gentler medication uptitration, early physical‑therapy referral, and regular medication reconciliation.
polypharmacy refers to the concurrent use of five or more medications magnifies adverse‑event risk. A quarterly review by a pharmacist or a geriatrician can pinpoint unnecessary drugs (e.g., nighttime sedatives) and replace them with safer alternatives. This practice also reduces drug‑drug interactions that could precipitate arrhythmias or renal injury.
Non‑Pharmacologic Interventions
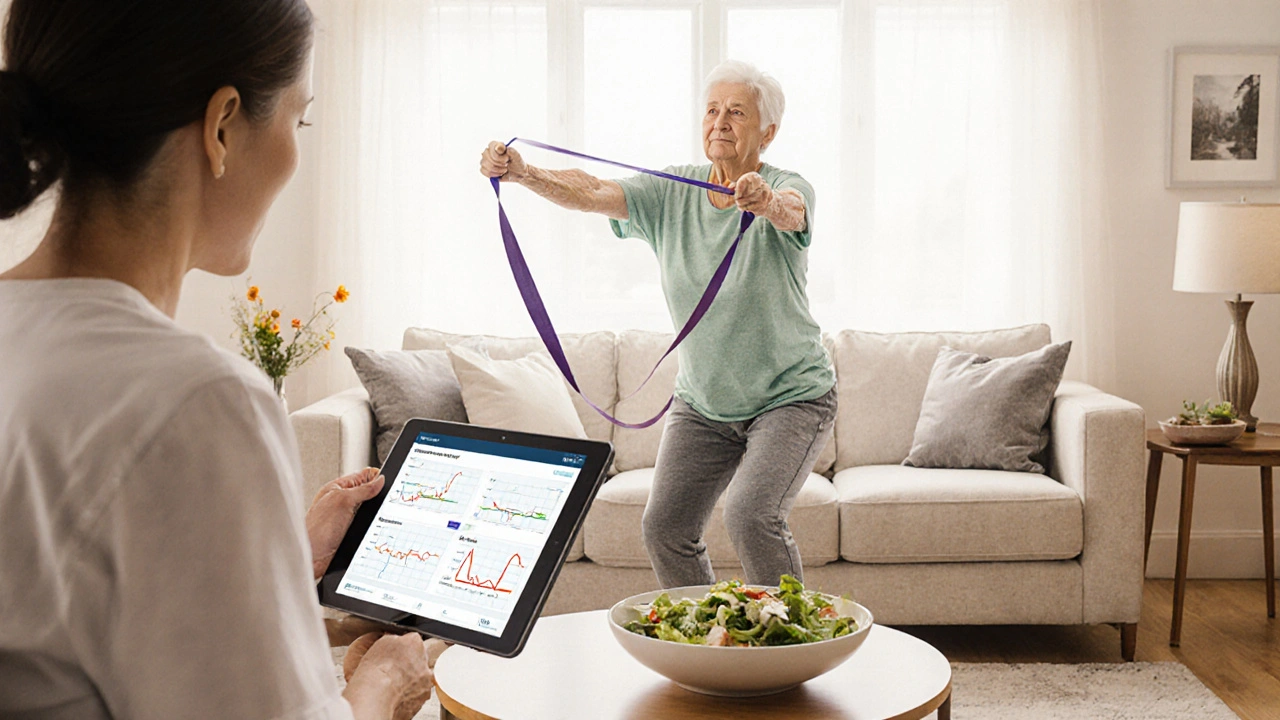
Exercise, nutrition, and technology play pivotal roles.
- Exercise: Even light resistance training twice a week improves muscle strength and can boost EF by up to 5% in frail seniors.
- Nutrition: A diet rich in lean protein (1.2g/kg body weight), low sodium (<2g/day), and adequate potassium supports cardiac function and mitigates diuretic‑induced electrolyte loss.
- telemonitoring uses remote sensors to track weight, blood pressure, and heart rhythm: Daily weight uploads combined with alerts for >2‑lb increases reduce hospital readmissions by 30% in the elderly cohort.
Palliative and End‑of‑Life Care
When symptom burden outweighs survival benefit, shifting focus to comfort is ethical and humane. palliative care provides relief from distressing symptoms while respecting patient goals includes low‑dose morphine for dyspnea, careful fluid management, and advance‑care planning. Engaging patients and families early ensures that interventions align with their values, whether that means staying at home or transitioning to hospice.
Comparison of Standard vs. Geriatric‑Adapted Heart‑Failure Therapy
| Aspect | Standard HF Therapy | Geriatric‑Adapted Therapy |
|---|---|---|
| Medication Dosing | Full guideline‑recommended doses | Start at 50% dose, titrate slowly |
| Monitoring Frequency | Every 4‑6weeks after titration | Every 2weeks during initial 3 months |
| Goal | Maximize survival and LV remodeling reversal | Preserve functional independence & reduce hospitalizations |
| Common Adjustments | Increase diuretic based on congestion | Consider low‑dose diuretic + electrolytes watch; limit ACE‑I if eGFR <30 |
| Additional Supports | Device therapy when indicated | Frailty screening, polypharmacy review, telemonitoring |
Practical Checklist for Clinicians
- Confirm diagnosis with age‑adjusted echo reference ranges.
- Assess frailty using the Fried criteria.
- Review all meds; discontinue non‑essential agents.
- Initiate ACE‑I or ARB at half dose; monitor renal function weekly for first 2weeks.
- Start beta‑blocker at 1.25mg; increase every 2weeks if heart rate >60bpm.
- Prescribe loop diuretic 20mg daily; adjust based on daily weight and potassium.
- Enroll patient in telemonitoring program if available.
- Discuss goals of care; document preferences for advanced interventions.
Frequently Asked Questions
Can an elderly patient tolerate full‑dose ACE inhibitors?
Often not. Starting at 50% of the guideline dose and titrating slowly while checking serum creatinine and potassium is safer. If eGFR falls below 30mL/min/1.73m², an ARB or low‑dose hydralazine‑nitrate combo may be preferred.
What are the red flags that indicate a need for palliative care?
Recurrent hospitalizations for fluid overload, intolerable side effects despite dose adjustments, severe frailty (e.g., unable to rise from a chair without assistance), and patient or family expressing desire for comfort‑focused treatment.
How often should weight be monitored at home?
Daily weighing at the same time, preferably after waking and before breakfast, gives the most reliable trend. An abrupt gain of 2lb (≈0.9kg) over 48hours should trigger a medication review.
Is cardiac resynchronization therapy (CRT) useful for seniors?
CRT can improve symptoms and reduce mortality in patients with reduced EF and wide QRS, even in those >80years, provided they have acceptable functional status and limited co‑morbidities.
What dietary sodium level is recommended?
Aim for less than 2grams (≈5g table salt) per day. Use herbs, lemon, and vinegar for flavor instead of salt.
By integrating these age‑specific tweaks, clinicians can improve survival, reduce hospital visits, and most importantly, keep older adults living with dignity. Remember, the focus isn’t just on the heart-it’s on the whole person.
heart failure elderly remains a pressing public‑health concern, but with thoughtful, individualized care, outcomes are getting better every day.

Picture this: an octogenarian stepping onto the clinic floor, heart thumping like a drumbeat of determination. The stakes are high, but with a “start low, go slow” mantra, we can tame that rebellious myocardium. Adjust ACE inhibitors to half the adult dose, keep a vigilant eye on potassium and creatinine – it’s the tightrope act that saves lives. Beta‑blockers? Initiate at a whisper, 1.25 mg, and let the body adapt before turning up the volume. And never forget the power of daily weight checks – a simple bathroom scale becomes a crystal ball for decongestion.
When we merge science with compassion, even the frailest heart can find its rhythm again.
Sure, because seniors totally love being tossed a full‑dose ACEi without a warning label, right?
Heart failure in the elderly isn’t just a textbook problem; it’s a daily drama where every lab value sings a different tune. First, recognize that arterial stiffening and reduced myocardial compliance turn a healthy pump into a creaky old engine. That’s why we must start ACE inhibitors at half the usual dose and watch the kidneys like a hawk – weekly creatinine and potassium checks become your new best friends. Beta‑blockers, those brave knights of the sympathetic realm, need to be introduced at a whisper of 1.25 mg, then nudged upward only if the pulse stays above 50 and the blood pressure doesn’t drop into the danger zone. Loop diuretics act as the stage crew, clearing excess fluid with a modest 20 mg of furosemide, while daily weight‑tracking provides the script for each act. If potassium threatens to rise above 5.5 mEq/L, pause the ACE inhibitor and consider a potassium‑binder or a switch to an ARB. For those with an eGFR under 30, the plot thickens – you might need to substitute hydralazine‑nitrate combos to keep the afterload low without harming the kidneys. Mineralocorticoid receptor antagonists add a subplot of mortality benefit, but only when potassium stays under 5.0 and eGFR stays above 30, otherwise the risk of hyperkalemia writes a tragic ending. Frailty scores, like the Fried phenotype, are the audience’s reactions – a high score signals you should rehearse dose adjustments more gently. Polypharmacy is the chorus of background voices; a quarterly pharmacist review can silence the discordant drug‑drug interactions before they steal the show. Exercise isn’t just a warm‑up; light resistance training twice a week can lift ejection fraction by up to five percent, a standing ovation for muscle strength. Nutrition, low‑sodium (<2 g) and protein‑rich (1.2 g/kg), fuels the body for the long performance ahead. When the curtain falls and symptoms overwhelm benefits, palliative care steps in, offering low‑dose morphine for breathlessness and a compassionate script for end‑of‑life wishes. Telemonitoring, the modern spotlight, can catch subtle weight gains of two pounds in 48 hours, prompting a timely diuretic tweak. Remember, the ultimate goal isn’t just to keep the heart beating, but to let the senior live with dignity, independence, and a smile on the final act.
Well, isn’t that just a masterclass in geriatric cardiology, complete with dosage titrations, electrolyte surveillance, and a sprinkle of frailty assessment; I must say, the thoroughness is impressive, though perhaps a tad overwhelming for the average practitioner, but hey, who doesn’t love a good checklist?; Your emphasis on daily weights, low‑salt diets, and even the occasional emoji‑free supportive note really ties the whole thing together, making it feel less like a protocol and more like a compassionate care plan; Keep it up, dear authors!
Great tips, especially the daily weight check.
Exactly! Monitoring weight daily is like having a tiny crystal ball 🔮 that tells you when fluid is building up. Pair that with a low‑sodium diet (think fresh herbs, not salt) and you give the heart a fighting chance. And don’t forget to celebrate each small win – a pound lost, a breath taken easier – those victories fuel the soul. 💪🏽 Stay bold, stay kind, and keep pushing those boundaries for our elders.
Start low, go slow, check labs, repeat – that’s the recipe. Also, definitely avoid big jumps in diuretic dose.
While your succinct mantra may appeal to those who favor brevity, it dangerously oversimplifies a nuanced clinical landscape that demands far more than a checklist without risking iatrogenic harm. The reality is that each elderly patient presents a unique constellation of comorbidities, polypharmacy interactions, and physiological changes that cannot be reduced to a checklist without risking iatrogenic harm. Ignoring the subtleties of renal function fluctuations, for instance, could lead to catastrophic hyperkalemia, especially when mineralocorticoid receptor antagonists are on board. Moreover, the nebulous instruction to “repeat” fails to specify the appropriate interval, which might be as frequent as weekly in the unstable phase, yet stretched to monthly once stability is achieved. Such ambiguity betrays an elitist confidence that the reader will intuit the missing details, a presumptuous stance that undermines patient safety. In short, your advice, though well‑intentioned, borders on dangerous minimalism, and the medical community would benefit from a more comprehensive, evidence‑based exposition rather than a terse slogan.
Oh sure, let’s just hand out full‑strength ACE inhibitors to every octogenarian and hope for the best 🙄💊.
That approach would likely increase adverse events rather than improve outcomes.
Honestly, most of this stuff is just rehashing what’s been known for decades; the real issue is the lack of adherence in our own healthcare system. We need tougher guidelines and stricter enforcement, not just gentle reminders. And let’s face it, the UK has been lagging behind the US in implementing these protocols efficiently. It’s high time we step up the game.
While I respect your point about systemic enforcement, I think a balanced approach works better – clear guidelines paired with supportive education ensures clinicians feel empowered rather than policed.
Thanks for the comprehensive overview; very helpful.