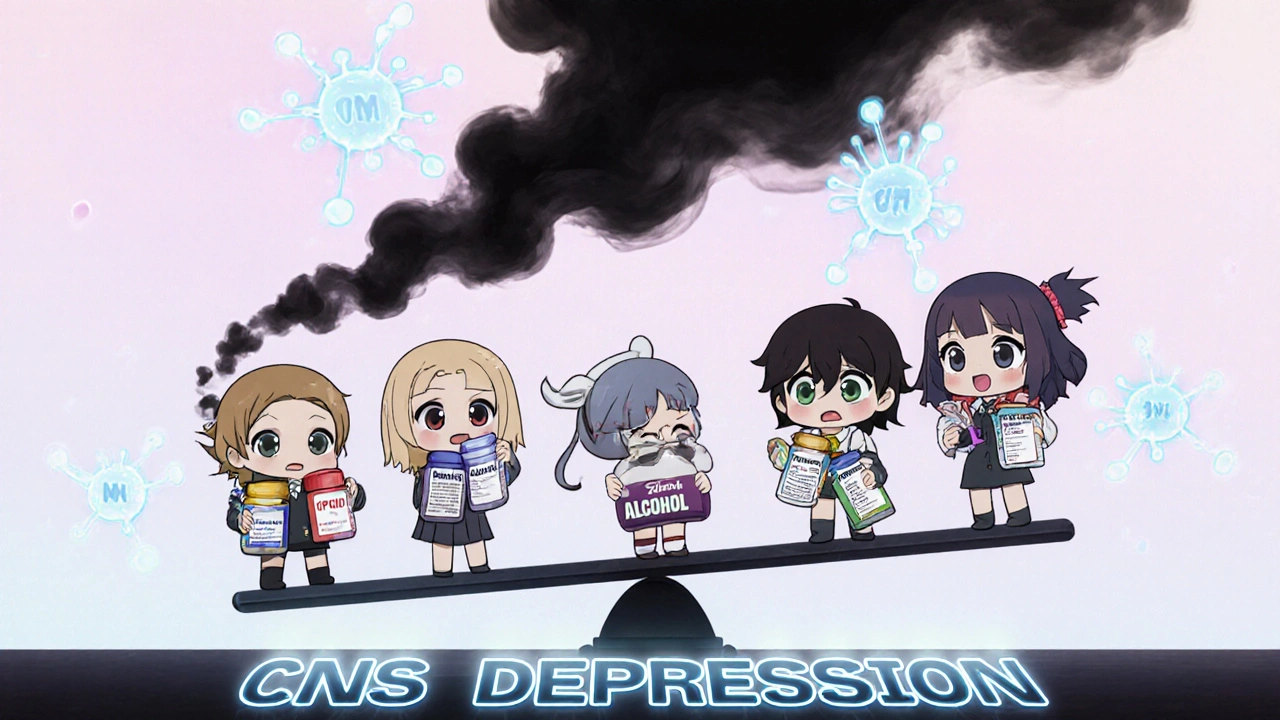
When you take one sedative, your body slows down a little. Take two, and it slows more. Take three or more - especially if they’re from different classes - and your brain and lungs can literally stop working. This isn’t a hypothetical risk. It’s happening right now, in homes, hospitals, and nursing facilities across the country. Combining sedatives like opioids, benzodiazepines, alcohol, or sleep pills doesn’t just add up - it multiplies danger in ways most people don’t expect.
What Happens When Sedatives Mix?
Sedatives work by boosting GABA, a neurotransmitter that tells your brain to chill out. That’s why they help with anxiety, insomnia, or seizures. But when you stack them - say, taking oxycodone for pain and alprazolam for anxiety - you’re not just doubling the effect. You’re triggering a synergistic crash in your central nervous system (CNS). This means your breathing slows dramatically, your heart rate drops, and your body loses the ability to wake up when oxygen levels fall. Studies show that mixing opioids with benzodiazepines increases the risk of fatal overdose by 2.5 to 4.5 times compared to using opioids alone. The FDA issued a formal warning in 2016 after reviewing hundreds of deaths linked to this combo. Even if you’re taking prescribed doses, the interaction doesn’t care about your doctor’s instructions - it only responds to chemistry. At the same time, alcohol - often overlooked as just a “social” drug - acts like another sedative. One drink with a sleep pill can drop your breathing rate from a normal 12-20 breaths per minute to 8-10. Two drinks? It can plunge to 4-6. That’s not sleep. That’s respiratory arrest waiting to happen.Who’s Most at Risk?
You might think this only affects people with substance use disorders. It doesn’t. The biggest group at risk? Older adults. Elderly patients are often prescribed multiple CNS depressants: one for arthritis pain (opioid), one for insomnia (zolpidem), one for anxiety (diazepam), and sometimes a muscle relaxant (cyclobenzaprine). All of these slow brain activity. The result? A 2.8 times higher risk of falls, 3.4 times more hip fractures, and a 27% increased chance of cognitive decline within a year. The American Geriatrics Society’s Beers Criteria lists 34 medications that should be avoided in seniors - many of them sedatives. Yet, studies show that 45% of elderly patients on three or more CNS-active drugs end up hospitalized for falls or confusion. And it’s not just age. Women are 1.7 times more likely to be prescribed these combinations. People with depression are over twice as likely. Higher opioid doses? That’s another red flag. Even younger adults aren’t safe. A 2020 CDC report found that 10.2% of people on long-term opioid therapy were still getting benzodiazepines prescribed alongside them - despite clear guidelines against it. Many patients don’t realize they’re combining dangerous drugs because their prescriptions come from different doctors, pharmacies, or specialties.The Silent Signs of Overdose
Most people think overdose means unconsciousness and blue lips. But the early signs are subtle - and often dismissed.- Slurred speech that’s “just tired”
- Confusion or forgetfulness that seems like aging
- Dizziness when standing up - blamed on low blood pressure
- Extreme drowsiness after meals or bedtime
- Slowed breathing - noticed by a partner but ignored as “normal snoring”
What You Can Do
The good news? This isn’t inevitable. There are proven ways to reduce risk. Start with a full medication review - every 3 to 6 months. Bring all your pills, supplements, and even over-the-counter sleep aids to your doctor. Don’t assume they know what you’re taking. Many patients don’t mention alcohol, marijuana, or herbal remedies like kava or valerian root - all of which can depress the CNS. Ask: “Are any of these drugs meant to calm my brain?” If the answer is yes, ask if they can be reduced or replaced. For anxiety, consider therapy or non-sedating medications like SSRIs (though even these can interact - more on that later). For sleep, try cognitive behavioral therapy for insomnia (CBT-I), which works better long-term than pills. If you’re on opioids, ask your doctor if you really need them. Chronic pain management doesn’t always require daily opioids. Non-opioid alternatives like gabapentin, physical therapy, or nerve blocks may be safer.What About Antidepressants?
Many people take SSRIs like sertraline or fluoxetine for depression. These aren’t sedatives - but they interfere with how your liver breaks down other drugs. About 69% of hospitalizations for depression involve multiple medications, and SSRIs can slow the metabolism of benzodiazepines, antipsychotics, and even some painkillers. This means even if you’re not taking a sedative directly, your SSRI might be making one last longer in your system. A 2022 study showed that combining SSRIs with CNS depressants increased suicide risk in vulnerable patients - not because SSRIs cause depression, but because they raise levels of other dangerous drugs in the blood. It’s not a reason to stop your antidepressant. But it’s a reason to ask your doctor for a drug interaction check - especially if you’re on more than two medications.
Technology Is Starting to Help
Some hospitals and clinics now use Clinical Decision Support (CDS) systems that flag dangerous combinations in real time. When a doctor tries to prescribe diazepam to someone already on hydrocodone, the system pops up a warning. In places where these systems are fully used, inappropriate sedative combinations dropped by 28%. By 2025, major electronic health record platforms like Epic and Cerner plan to make these alerts mandatory. That’s a big step. But it won’t fix everything. Many people get prescriptions from multiple providers who don’t share records. That’s why personal vigilance still matters.What to Do If You’re Already on Multiple Sedatives
If you’re currently taking two or more CNS depressants, don’t stop suddenly. Withdrawal from benzodiazepines or opioids can cause seizures, hallucinations, or even death. Instead:- Write down every medication, supplement, and substance you take - including alcohol, marijuana, and sleep aids.
- Bring that list to your primary care doctor or pharmacist.
- Ask: “Which of these are absolutely necessary? Which can be reduced or replaced?”
- Request a deprescribing plan - a slow, monitored taper of one drug at a time.
The Bottom Line
Combining sedatives isn’t just risky - it’s deadly. And it’s happening more often than you think. The drugs themselves aren’t evil. But when stacked without oversight, they turn into silent killers. You don’t need to be an addict. You don’t need to be reckless. You just need to know that your “normal” medication routine could be putting your life at risk. Ask questions. Review your pills. Talk to your doctor. Your breathing - and your life - depend on it.Can I mix alcohol with my sleep medication?
No. Mixing alcohol with any sedative - whether it’s zolpidem, eszopiclone, or benzodiazepines - dramatically increases the risk of respiratory depression. Even one drink can slow your breathing to dangerous levels, especially at night when your body is already resting. Emergency rooms see this combination often. It’s not worth the risk.
Are over-the-counter sleep aids safe to combine with prescription sedatives?
No. Many OTC sleep aids like diphenhydramine (Benadryl) or doxylamine (Unisom) are antihistamines that have strong sedative effects. They work on the same brain pathways as prescription drugs. Combining them can lead to excessive drowsiness, confusion, and slowed breathing - even if you take them hours apart. There’s no safe window.
What should I do if I think someone is overdosing on sedatives?
Call 911 immediately. Look for slow or irregular breathing, unresponsiveness, blue lips or fingertips, and extreme drowsiness. Do not wait to see if they “sleep it off.” Administer naloxone if available and you suspect opioids are involved, but remember: naloxone won’t reverse benzodiazepine or alcohol overdose. Emergency care is still needed.
Can I take CBD with my anxiety medication?
CBD can interact with many CNS depressants by inhibiting liver enzymes that break them down. This can cause higher levels of your medication to build up in your blood - increasing sedation and risk of overdose. If you’re on benzodiazepines, opioids, or sleep aids, talk to your doctor before using CBD. It’s not automatically safe just because it’s “natural.”
Is it safe to take two different benzodiazepines together?
No. Taking two benzodiazepines - like lorazepam and clonazepam - together multiplies the risk of CNS depression without adding any therapeutic benefit. This is called “stacking,” and it’s a common mistake. Your doctor should prescribe only one at a time, and only if absolutely necessary. Never combine them without explicit medical supervision.
Why do doctors still prescribe these combinations if they’re so dangerous?
Many doctors are unaware of the full risk or feel pressured to treat multiple symptoms quickly. Patients with chronic pain and anxiety often get separate prescriptions from different specialists. Without a full medication review, dangerous overlaps slip through. That’s why it’s critical for you to speak up - and ask for a coordinated care plan.
Can pharmacogenomic testing help prevent dangerous combinations?
Yes. Some people have genetic variations in liver enzymes (like CYP2D6 or CYP3A4) that make them poor metabolizers of certain drugs. This means sedatives stay in their system longer, increasing overdose risk. Testing can identify these individuals and help doctors choose safer alternatives. While not yet routine, it’s becoming more accessible and could reduce dangerous interactions by up to 22% in high-risk groups.

This is terrifying. I didn’t realize my grandma’s nightly glass of wine with her sleeping pill was basically playing Russian roulette with her breathing.
As a pharmacist, I see this every week. People think OTC means safe. It doesn’t. Diphenhydramine + benzos + alcohol? That’s a death cocktail disguised as self-care. Please, bring your full med list to the pharmacy - we’ll catch what the doctor misses. I’ve saved lives this way.
Look, I get it - doctors are overworked, patients are anxious, and everyone wants a quick fix. But stacking sedatives isn’t just dangerous - it’s lazy medicine. I’ve seen elderly patients on five different CNS depressants because each specialist treated one symptom in isolation. No one looked at the whole picture. The system is broken. We need integrated care teams, not siloed prescriptions. And yes, that means more time, more coordination, more cost - but not more dead grandmas. CBT-I works better than zolpidem long-term. SSRIs are safer than benzos for anxiety. We know this. Why aren’t we doing it?
Also, people forget that kava, valerian, and even some CBD oils are CNS depressants. They’re not regulated. No FDA oversight. No warning labels. Just a bottle on a shelf with a pretty picture. That’s not natural health - that’s pharmacological roulette.
And don’t get me started on the myth that ‘I only take it once in a while.’ Timing doesn’t matter. Accumulation does. Your liver doesn’t care if you drank at 8 PM or 11 PM. It metabolizes what’s there. And if you’re on an SSRI? That metabolism slows down. Suddenly, one drink becomes three. One pill becomes five. And your brain? It just stops.
Deprescribing isn’t about taking away comfort. It’s about replacing danger with dignity. My uncle tapered off clonazepam over six months with a geriatric psychiatrist. He sleeps worse at first - but he hasn’t fallen in a year. His cognition improved. He started gardening again. That’s the real win. Not the pill. The life.
We need to normalize asking: ‘Is this still necessary?’ Not ‘Can I take one more?’
The tragedy isn't the drugs... it's the illusion of control. We think we're managing our lives by stacking sedatives - but really, we're outsourcing our pain, our anxiety, our insomnia - to chemistry. And chemistry? Chemistry doesn't care about your intentions. It doesn't know your name. It doesn't remember your doctor's note. It just reacts. And when it reacts, it doesn't ask permission. It just... stops. The real question isn't 'how many?' - it's 'why are we so desperate to quiet our minds that we're willing to silence our breath?'
The 2.8x fall risk stat? That's the tip of the iceberg. The real cost is the institutionalization. Elderly patients on poly-sedatives end up in nursing homes not because they're frail - because they're drugged. And the system profits from that. Pharma makes money. Hospitals get reimbursed. Families feel guilty. Everyone loses except the machine.
You're all missing the point. The FDA warning in 2016? That was after 1,200+ deaths. But the real problem is off-label prescribing. Most people on this combo aren't even told it's dangerous. Doctors say 'take this for sleep' and 'take this for pain' and never connect the dots. And patients? They're too scared to ask. I've seen patients on 7 CNS drugs - all prescribed by different MDs - and none of them knew what each one did. It's not negligence. It's systemic ignorance. And until EMRs auto-flag every interaction - not just opioids and benzos - this will keep happening.
There’s a quiet kind of courage in asking, ‘Do I really need this?’ Most people don’t have the energy - or the access - to question their prescriptions. But that question? It’s the first step back from the edge. Not every ache needs a chemical answer. Not every sleepless night needs a pill. Sometimes, it just needs someone to sit with you in the dark and say, ‘I’m here.’ That’s the medicine we’ve forgotten how to give.
And yeah - naloxone won’t fix a benzo overdose. But compassion? That always works.
So let me get this straight - we’ve got a system that prescribes 5 sedatives to old people, then blames them for falling? And we call that healthcare? Cool. Real cool. Next they’ll blame the oxygen for being too low.
This is why America is falling apart. We got too many pills, too many doctors, and no accountability. My aunt took 3 benzos, an opioid, and melatonin - and they said she 'just had a stroke.' No, she had polypharmacy. And no one wants to admit it. We need to stop treating symptoms and start treating PEOPLE. Also, why are we letting CBD be sold like candy? It's not a supplement - it's a drug. Regulate it or ban it.
The data is clear. The risk is exponential. The solutions exist. So why does this keep happening? Because the system rewards volume over safety. Prescribe more. Bill more. Repeat. It's not a medical failure. It's a financial one.
just stop mixing stuff. your body isn't a cocktail bar.
It's not just dangerous - it's negligent. Prescribing multiple CNS depressants without a coordinated review is malpractice. Every physician has a duty to assess drug interactions. Failure to do so is not an oversight - it's a breach of the standard of care. If your doctor hasn't reviewed your full medication list in the last six months, you need a new doctor. Period.