Type 2 Diabetes: Causes, Management, and What You Need to Know
When your body stops responding properly to insulin, a hormone that helps move sugar from your blood into your cells. Also known as insulin resistance, it’s the core problem behind type 2 diabetes, a chronic condition where blood sugar stays too high over time. This isn’t just about eating too much sugar—it’s about how your body handles fuel, how your pancreas keeps up (or doesn’t), and what happens when that system breaks down over years.
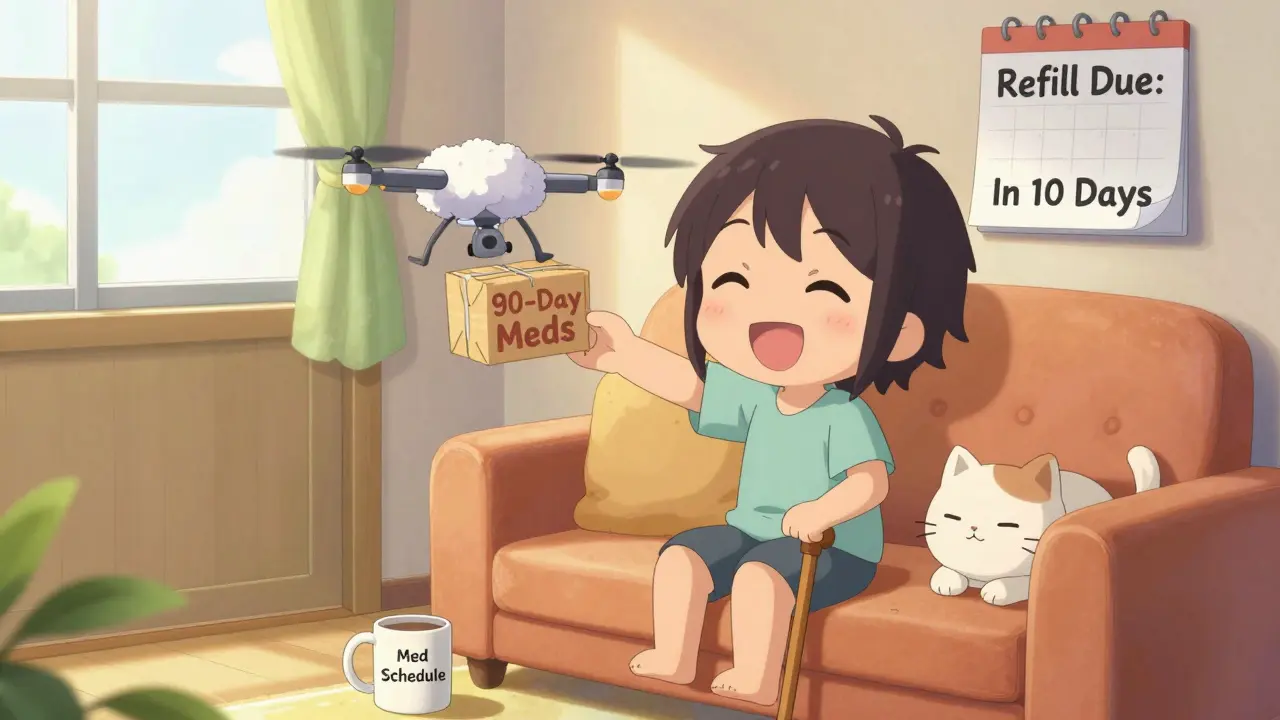
Many people with type 2 diabetes don’t feel sick at first. That’s why it often goes undiagnosed until complications show up—nerve damage, vision issues, or heart problems. But the good news? It’s not inevitable. Lifestyle changes like losing even 5% of body weight, walking 30 minutes a day, and cutting back on processed carbs can reverse early-stage insulin resistance. For others, medication becomes necessary. Drugs like metformin, GLP-1 agonists, and SGLT2 inhibitors don’t just lower blood sugar—they can protect your heart and kidneys, too. These aren’t one-size-fits-all options. What works for one person might not work for another, and that’s why understanding your own body’s response matters more than following a generic plan.
It’s easy to get overwhelmed by the flood of advice: keto? intermittent fasting? supplements? But the real focus should be on consistency, not perfection. Regular blood sugar checks, knowing how your body reacts to food and stress, and working with your doctor to adjust meds over time are the keys that actually move the needle. You’ll find posts here that compare common diabetes medications, explain how certain drugs affect your heart, and even break down what to do when lifestyle changes aren’t enough. There’s no magic pill, but there are proven paths—and they start with understanding what’s really going on inside your body.