When menopause hits, your body changes. Hormones drop. Hot flashes spike. Sleep vanishes. Vaginal dryness makes sex painful. Mood swings feel like a storm you didn’t sign up for. For many women, these aren’t just inconveniences-they’re life-altering. That’s why millions turn to hormone therapy. But here’s the thing: medications during menopause don’t just fix symptoms. They change how your body reacts to everything else. Side effects shift. Risks flip. What worked last year might not be safe this year.
What Hormone Therapy Actually Does
Menopause hormone therapy (HRT) replaces estrogen, and sometimes progesterone, that your ovaries stop making. It’s not a magic bullet. It’s a tool. Used right, it can slash hot flashes by 70-80%. It can stop bone loss. It can make sex comfortable again. But it’s not the same for everyone.
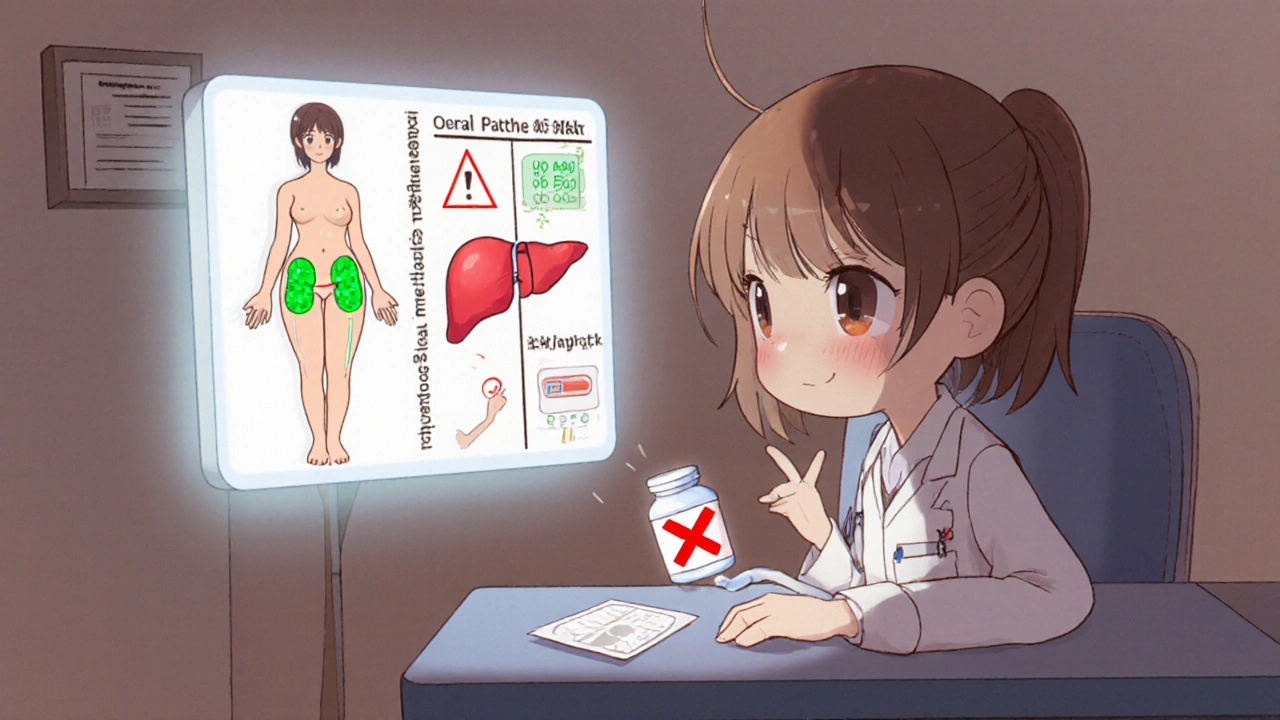
Estrogen-only therapy is for women who’ve had a hysterectomy. If you still have a uterus, you need progesterone too-or your risk of uterine cancer goes up. That’s why most women get combination therapy: estrogen plus progestin. Pills like Duavee (conjugated estrogen + bazedoxifene) are designed to protect the uterus without extra progesterone. Patches, gels, and vaginal rings deliver hormones through the skin or local tissue, avoiding the liver entirely. That matters. Oral pills increase clot risk. Patches don’t. The difference isn’t small-it’s life-changing.
The Real Risks: Numbers That Matter
Let’s cut through the noise. You hear "HRT raises breast cancer risk." But what does that actually mean?
For every 10,000 women taking combination HRT for five years, about 30 develop breast cancer naturally. With HRT, that number jumps to 38. That’s 8 extra cases. Not 80. Not 800. Eight. Same with stroke: from 21 to 29 cases per 10,000 women. Blood clots? From 10 to 18. These aren’t trivial. But they’re not inevitable.
Age and timing change everything. If you start HRT before 60 or within 10 years of your last period, your heart risk doesn’t rise-it may even drop. Women who wait until 70? Their stroke risk climbs 24% higher than those who started early. The FDA warns about dementia in women over 65, but that’s mostly linked to starting therapy late. The window matters. The clock ticks.
Side Effects You Can’t Ignore (And Which Ones Fade)
Not all side effects are scary. Some are just annoying. And most fade.
Spotting or bleeding? Happens in 30-50% of women in the first 3-6 months. It’s not cancer. It’s your lining adjusting. If it keeps going past six months, talk to your doctor. Breast tenderness? 20-30% of users feel it. Usually gone in a month. Bloating? Fluid retention affects 15-25%. Headaches? 10-20%. Nausea? 15-20%. These aren’t signs you’re breaking. They’re signs your body is adapting.
But some red flags don’t fade. Sudden chest pain? Trouble breathing? Swelling in one leg? Vision loss? Severe headache? These aren’t side effects. These are emergencies. Call your doctor. Now. The risk of blood clots doubles or triples with oral estrogen. Patches cut that risk by 30-40%. That’s why more women are switching.
What Works When Hormones Don’t
Not everyone can take hormones. Cancer history? Blood clots? Stroke? Liver disease? Then HRT is off the table. But you still have options.
SSRIs like paroxetine? They reduce hot flashes by 50-60% in 60% of users. Gabapentin? Lowers them by 45%. Clonidine? 46%. These aren’t perfect, but they work. Vaginal dryness? Over-the-counter moisturizers help 45% of women. DHEA inserts like Intrarosa? Improve pain during sex in 70% of users-with almost no hormone entering your bloodstream.
And then there’s fezolinetant. New. FDA-reviewed. In trials, it cut moderate-to-severe hot flashes by over 50%. No estrogen. No progesterone. Just a pill targeting brain signals that trigger flushes. Coming soon. It’s the future.
How to Adjust When Things Go Wrong
Side effects don’t mean you quit. They mean you tweak.
68% of women find relief just by changing the dose. Too much estrogen? Your breasts hurt. Too little? Hot flashes return. A 50% reduction in dose can make all the difference. Switching from a pill to a patch? Reduces nausea and bloating by 60%. Moving from daily to every-other-day? Stops spotting. A 2021 study found most women get it right after one or two adjustments.
Missed a pill? Don’t double up. Take it as soon as you remember. If it’s almost time for the next one? Skip it. Double doses raise clot risk. And never mix HRT with other estrogen or progestin pills. Duavee users who did? 12% had bad interactions.

Who Should Avoid Hormone Therapy Altogether
Some women simply shouldn’t take it. If you’ve had:
- Breast cancer
- Endometrial cancer
- Stroke or heart attack
- Deep vein thrombosis or pulmonary embolism
- Active liver disease
Then HRT is dangerous. Period. Even low-dose vaginal estrogen? Avoid it if you’ve had estrogen-sensitive cancer. Your doctor will know. They’ll check your history. They’ll ask about family risk. Don’t skip that part.
And if you’re over 65? The risks of dementia and stroke climb. The benefits? Slim. For memory, sleep, or mood? Try therapy, exercise, or non-hormonal meds first.
What About Herbal Remedies?
Black cohosh? Red clover? Soy isoflavones? They’re everywhere. But here’s the truth: 12 clinical trials involving nearly 2,000 women found mixed results. Some saw mild relief. Most saw nothing. And no one knows the long-term safety. The FDA doesn’t regulate supplements. One batch might be clean. Another might be laced with estrogen. Don’t gamble with your health.
Herbs aren’t safer. They’re untested. Stick to what’s studied. What’s approved. What’s tracked.
Where Do You Go From Here?
Menopause isn’t a disease. But it’s a medical event. And like any medical event, it needs a plan.
Start with your doctor. Not a blog. Not a friend. Not a social media post. Talk about your symptoms. Your history. Your fears. Ask: "Is HRT right for me now?" "What’s my personal risk for blood clots?" "Could a patch work better than a pill?"
Don’t accept "it’s just menopause" as an answer. You deserve relief. You deserve safety. You deserve options that match your body-not someone else’s.
There’s no one-size-fits-all. But there is a right path-for you. And it starts with asking the right questions.
Can hormone therapy cause weight gain during menopause?
Hormone therapy doesn’t directly cause weight gain. The weight gain most women experience during menopause comes from aging, slower metabolism, and muscle loss-not estrogen. Some women report bloating from fluid retention, especially with oral pills, but this usually clears up in a few weeks. Patches and gels are less likely to cause this. If you’re gaining weight, focus on diet, strength training, and sleep-not stopping HRT.
How long should I stay on hormone therapy?
There’s no fixed timeline. Most women take HRT for 2-5 years to manage symptoms. But if you’re still having severe hot flashes or bone loss at age 60, continuing may still make sense. The key is reevaluating every year. Talk to your doctor. Check your risk factors. If your symptoms are gone and your bone density is stable, you might taper off. If they’re not? Staying on low-dose therapy is often safer than letting symptoms damage your sleep, mood, or relationships.
Are natural or bioidentical hormones safer than traditional HRT?
No. "Bioidentical" hormones made in compounding pharmacies aren’t FDA-approved. They’re not tested for safety, purity, or dosing accuracy. The same risks apply: blood clots, stroke, breast cancer. The FDA and ACOG warn against them. If a pharmacy tells you they’re safer, they’re wrong. Stick to FDA-approved pills, patches, or gels. They’re monitored. They’re studied. They’re predictable.
Can I use HRT if I have a family history of breast cancer?
It depends. If you have a BRCA mutation or strong family history, your risk is higher. But not all HRT is equal. Estrogen-only therapy (if you’ve had a hysterectomy) carries less risk than combination therapy. Patches may be safer than pills. Your doctor can run a risk assessment using tools like the Gail model. For some women with family history, non-hormonal options like SSRIs or fezolinetant are better. Never assume HRT is off-limits-ask for a personalized plan.
Do I need to get regular mammograms while on HRT?
Yes. All women over 50 should get mammograms every 1-2 years, regardless of HRT use. But if you’re on combination hormone therapy, your breast density may increase, making mammograms harder to read. Your radiologist needs to know you’re on HRT. Some doctors recommend an annual mammogram for HRT users. Don’t skip screenings. Early detection saves lives.
What if I start HRT and feel worse?
Don’t panic. Many side effects-headaches, bloating, mood swings-get better in 2-3 months. But if you feel worse after six weeks, talk to your doctor. You might need a lower dose, a different type of estrogen, or a patch instead of a pill. About 45% of women who switch delivery methods see improvement. Don’t suffer through it. Adjustments work. You just need to speak up.
Can HRT help with depression during menopause?
For some women, yes. Mood swings and depression during menopause are often tied to hormone drops. Estrogen helps regulate serotonin, the mood chemical. If your depression is linked to hot flashes, night sweats, or sleep loss, HRT can help by fixing those triggers. But if you have clinical depression, HRT alone won’t be enough. You’ll likely need therapy or antidepressants. HRT can be part of the solution-but not the whole answer.
Is there a link between HRT and gallbladder disease?
Yes. Oral estrogen increases bile cholesterol, raising the risk of gallstones. The FDA says HRT can increase gallbladder disease risk by 77%. This is mostly true for pills, not patches or gels. If you have a history of gallstones, ask your doctor about transdermal options. Symptoms like upper right belly pain, nausea after fatty meals, or bloating should be checked. Don’t ignore it-gallbladder attacks can be serious.



Wow, this is one of the clearest breakdowns of HRT I’ve ever read-seriously, thank you. I was terrified of starting it after reading scary headlines, but seeing the actual numbers (38 vs. 30 per 10k) made me feel way more in control. Also, the patch vs. pill difference? Game-changer. I switched last year and my bloating vanished. No more 3 p.m. panic attacks about clots.
It is of paramount importance to underscore the nuanced nature of hormonal intervention during the menopausal transition, as the physiological alterations wrought by declining ovarian function are not monolithic nor uniformly experienced across the demographic spectrum. Furthermore, the temporal window hypothesis, as elucidated by the Women’s Health Initiative and corroborated by subsequent longitudinal analyses, posits that initiation of hormone therapy within the first decade following the final menstrual period confers a significantly more favorable risk-benefit profile than delayed commencement, particularly with regard to cardiovascular outcomes and cognitive preservation. Consequently, clinicians are ethically obligated to engage in individualized risk stratification, incorporating not only personal and familial medical histories but also biomarkers of metabolic health, inflammatory status, and vascular integrity, before prescribing any form of exogenous estrogen or progestin.
Y’all overcomplicating this. I took the patch, got hot as hell for 2 weeks, then boom-peace. No more crying over spilled coffee. 🤷♂️ If your doc ain’t listening, find a new one. Period.
Menopause isn’t a flaw to fix. It’s a transition. But if you’re suffering? You deserve relief. No guilt. No shame. HRT isn’t weakness-it’s wisdom. I’ve seen women go from barely sleeping to hiking mountains again. Just don’t let fear decide for you. Talk to someone who gets it. 🌱
Why are we even giving women hormones? This is just Big Pharma pushing pills. In my grandma’s day, women just dealt with it. No pills, no drama. Now we’ve turned a natural phase into a medical crisis. And don’t even get me started on these ‘bioidentical’ scams. Wake up, America.
I started HRT at 52 after 18 months of sleepless nights and mood swings that made me cry during Zoom calls. Patch. Low dose. Took 3 weeks. Now I sleep. I laugh. I don’t hate my husband anymore. Best decision I ever made. No regrets.
Why are we still talking about estrogen like its some kind of miracle drug? I’ve been on it for 3 years and I still get headaches every damn week. My doctor says it’s normal. I say it’s not worth it. I’m done. Time to try yoga or something
Man, I love how this post doesn’t just throw numbers at you-it tells you what they mean. Like, 8 extra breast cancer cases per 10k? That’s less than the risk from drinking a glass of wine daily. And patches cutting clot risk by 30-40%? That’s the kind of info you need to actually make a choice. Kudos. Also, fezolinetant sounds like sci-fi. I’m already waiting for my prescription.
Ugh. Another woman falling for the hormone trap. You think you’re ‘empowered’ taking pills but you’re just letting Big Pharma control your body. My mom went through menopause in the 70s-no meds, no drama. She lived to 92. You’re all just scared of aging. Grow up.
One must acknowledge the epistemological limitations of contemporary endocrinology when discussing menopausal interventions. The reductionist paradigm that equates symptom relief with therapeutic success fails to account for the phenomenological depth of the menopausal experience-often dismissed as mere ‘biological malfunction’ rather than a profound ontological shift. Moreover, the commodification of hormonal therapy as a panacea obscures the sociocultural anxieties surrounding female aging. One wonders: are we treating symptoms-or reinforcing patriarchal norms of youthful vitality?
I’m 58 and started HRT at 54. I didn’t tell anyone. I was ashamed. But now I’m sleeping through the night and my anxiety is gone. I still feel weird talking about it. Why is this so hard to say out loud? I just wish I’d known how normal it was to need help.
For anyone considering HRT: if you’re still having hot flashes after 6 months off, don’t assume it’s ‘just menopause.’ Talk to a menopause specialist, not your GP. There’s a whole field called NAMS-certified providers. They know the difference between a patch and a pill. And yes, vaginal DHEA? It’s not magic-but it’s real. And it saved my sex life.
My wife started HRT after 18 months of hell. She’s back to gardening, laughing, even dancing again. I didn’t get it at first. Thought she was being dramatic. Turns out, I was the one who didn’t understand. Thanks for this post-it’s like a map for people lost in the fog.