Why Lung Cancer Screening Matters More Than Ever
Most people don’t realize that lung cancer kills more people each year than breast, colon, and prostate cancer combined. The biggest reason? It’s often found too late. When caught in stage IV, only about 6% of patients survive five years. But if it’s caught early-before it spreads-survival jumps to nearly 60%. The problem isn’t lack of knowledge. It’s lack of action. Only 23% of lung cancer cases are found early. That’s not because the tools don’t exist. They do. And they’re getting better.
Who Should Be Getting Screened?
If you’re a current or former smoker, you’re in the high-risk group. But not all guidelines agree on who qualifies. The U.S. Preventive Services Task Force (USPSTF) says you should get screened annually if you’re between 50 and 80, have smoked at least 20 pack-years, and either still smoke or quit within the last 15 years. A pack-year means smoking one pack a day for a year. So 20 pack-years could be one pack daily for 20 years, or two packs a day for 10 years.
But here’s the twist: the American Cancer Society updated its guidelines in 2023 and removed the 15-year quit limit entirely. That means if you smoked 20 pack-years and quit 20 years ago, you still qualify. Why? Because research shows your risk stays high for decades. A 2022 study in JAMA Oncology found former smokers 15 to 30 years out still had 2.5 times the risk of lung cancer compared to people who never smoked.
The American Association for Thoracic Surgery takes a different approach. They require 30 pack-years for most people, but allow screening starting at age 50 if you have a 20 pack-year history plus other risk factors-like family history, asbestos exposure, or chronic lung disease. Medicare follows the USPSTF rules: coverage starts at 50, requires 20 pack-years, and ends at 77. Many private insurers haven’t caught up yet. Some still require 30 pack-years and age 55+, leaving thousands without access.
How Screening Works: Low-Dose CT Scans
The only proven method for early lung cancer detection is low-dose computed tomography, or LDCT. It’s not a regular CT scan. It uses 70-80% less radiation-about the same as a mammogram. The machine takes detailed cross-sections of your lungs in seconds. No needles, no fasting, no prep. You just lie on a table, hold your breath for 10 seconds, and it’s over.
But here’s the catch: LDCT finds a lot of things that aren’t cancer. In fact, 96% of positive scans turn out to be false alarms. That’s not a flaw-it’s expected. The goal isn’t perfection. It’s catching the real cancers early. Still, false positives lead to unnecessary biopsies, anxiety, and extra costs. That’s why screening must be done at accredited centers with experienced teams who know how to interpret results correctly.
Not all clinics are created equal. Only about 2,800 facilities in the U.S. are accredited by the American College of Radiology for lung cancer screening. Rural areas have 67% fewer of these centers than cities. If you live outside a major metro, getting screened might mean driving hours. And even if you get the scan, follow-up care isn’t guaranteed. A 2021 study found only 45-60% of eligible people stick with annual screening. Missed scans mean missed chances.
The Big Gap: Why So Few People Get Screened
There are 14.5 million Americans who meet current screening criteria. But in 2021, only 2.6 million actually got screened. That’s less than 18%. Why?
- Doctors don’t bring it up. A 2022 AMA survey found 42% of primary care doctors didn’t even know about the updated USPSTF guidelines.
- Patients don’t know they’re eligible. Many think only heavy smokers or people with symptoms need screening. But lung cancer often has no early symptoms.
- Insurance confusion. Medicare covers it. But some private plans still use old rules. If your insurer says you don’t qualify, ask for a copy of their policy. You might be eligible under federal law.
- Racial and geographic disparities. Black smokers are 35% less likely to be screened than white smokers. Rural residents face even steeper access barriers.
Successful programs fix this with simple tools: electronic health record alerts that pop up when a patient meets criteria, patient navigators who help schedule scans, and integrated smoking cessation programs. One study showed EHR prompts boosted screening rates by 32%. Another found patient navigators improved follow-up by 27%.
Targeted Therapy: Turning Early Detection Into Long-Term Survival
Screening finds cancer early. But finding it isn’t enough. Treatment matters. And here’s where things have changed dramatically.
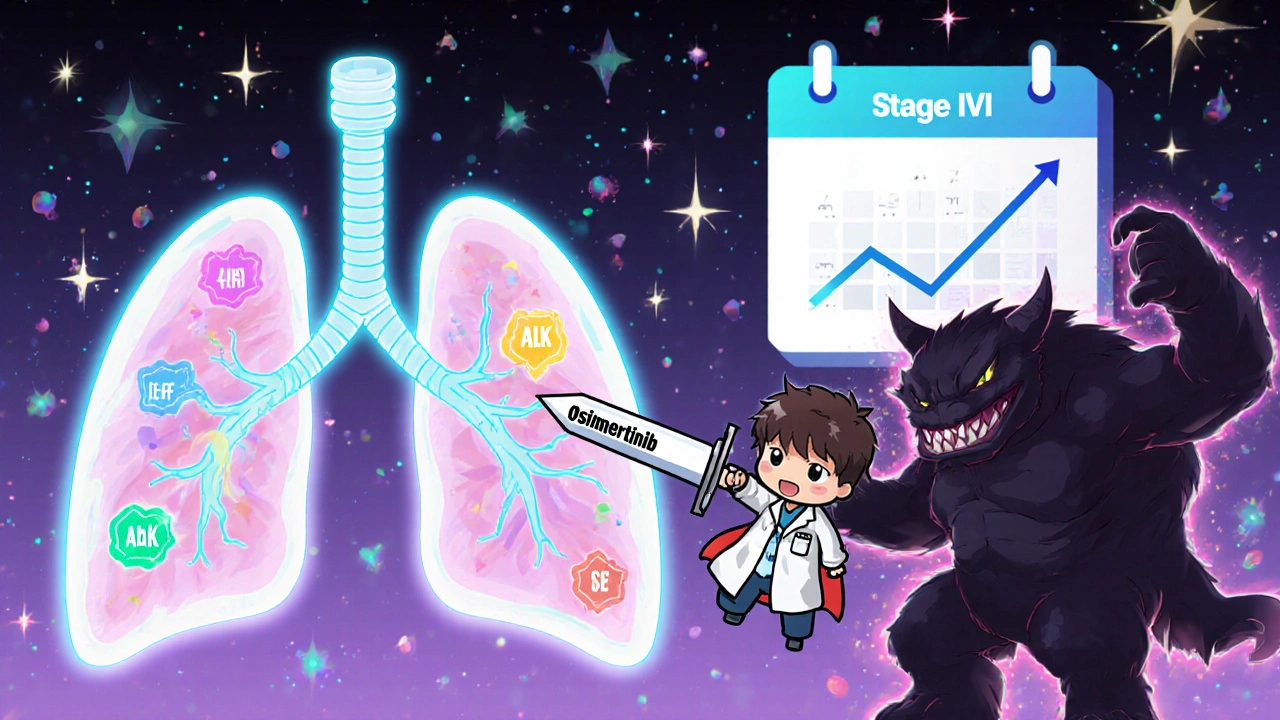
For decades, lung cancer treatment meant surgery, chemo, and radiation. Now, for about 30% of patients with non-small cell lung cancer (NSCLC), there’s a better option: targeted therapy. These drugs attack specific genetic mutations in the tumor-like EGFR, ALK, ROS1, or KRAS-without wrecking healthy cells.
The biggest breakthrough? Osimertinib (Tagrisso). In 2020, the FDA approved it as an adjuvant treatment for early-stage NSCLC patients with EGFR mutations after surgery. The ADAURA trial showed it cut the risk of cancer returning or spreading by 83%. That’s not just survival. That’s a near-normal life expectancy for many.
Here’s the connection: screening finds cancer early, when it’s still localized. That’s when targeted therapies work best. By 2025, experts predict 70% of early-stage lung cancers found through screening will have actionable mutations-compared to only 30% in late-stage cases. That means screening isn’t just about catching cancer. It’s about catching cancer that can be cured with pills.
Future tests are even more promising. Liquid biopsies-blood tests that detect tumor DNA-are being tested in trials like NCT04541082. The idea? Find cancer signals in your blood before a tumor shows up on a CT scan. If it works, we could be detecting lung cancer years earlier, even before smoking damage becomes visible.
What’s Next: AI, Risk Models, and Personalized Screening
Screening isn’t one-size-fits-all anymore. New tools are making it smarter.
The FDA approved LungQ by Riverain Technologies in January 2023-the first AI software designed to help radiologists interpret lung scans. In trials, it reduced unnecessary follow-up scans by 22% by better distinguishing real tumors from benign nodules.
The National Cancer Institute is launching the PACIFIC trial in 2024, testing whether adding genetic risk scores and environmental exposures (like radon or air pollution) can improve who gets screened. Right now, we screen based on smoking history alone. But what if we could identify a 45-year-old who smoked 15 pack-years but has a high genetic risk? They might need screening too.
By 2030, experts believe lung cancer screening programs will routinely combine LDCT with genetic risk models and liquid biopsy screening. The goal? Raise the five-year survival rate from today’s 23% overall to over 40% by catching cancer early and treating it precisely.
What You Can Do Right Now
If you’re a current or former smoker:
- Calculate your pack-years. Multiply the number of packs you smoked per day by the number of years you smoked.
- Check your age. If you’re 50 or older and have 20+ pack-years, you qualify under the newest guidelines.
- Ask your doctor: “Am I eligible for lung cancer screening?” Don’t wait for them to bring it up.
- If you still smoke, ask about quitting support. Screening programs should include cessation counseling. Over 70% of smokers want to quit-but only 30% get help.
- If your insurance denies coverage, ask for a copy of their policy. You may be eligible under federal rules.
Early detection saves lives. But only if you act. Screening isn’t a luxury. It’s a lifeline-for you, and for the people who love you.
Who qualifies for lung cancer screening?
You qualify if you’re between 50 and 80 years old, have smoked at least 20 pack-years (one pack a day for 20 years, or equivalent), and currently smoke or quit within the last 15 years. The American Cancer Society now recommends screening even if you quit more than 15 years ago, as long as you have a 20+ pack-year history. Some groups, like the American Association for Thoracic Surgery, also allow screening for younger people with additional risk factors like family history or asbestos exposure.
Is lung cancer screening covered by insurance?
Yes, under federal law, Medicare and most private insurers must cover annual low-dose CT (LDCT) screening for eligible individuals under the Affordable Care Act. Medicare covers it for people aged 50-77 with a 20+ pack-year history who currently smoke or quit within the past 15 years. Some private insurers still use outdated rules requiring 30 pack-years or age 55+. If you’re denied, ask for their policy in writing-you may be eligible under the 2021 USPSTF guidelines.
What if my scan shows a nodule?
Most lung nodules are not cancer-about 96% of positive screens are false positives. But any nodule needs follow-up. Your care team will monitor its size and shape over time with repeat scans, usually at 3, 6, or 12 months. If it grows or looks suspicious, you may need a biopsy. Accredited screening centers have protocols to avoid unnecessary procedures. Don’t panic. Follow your doctor’s plan.
Can non-smokers get screened?
Current guidelines focus on smokers and former smokers because they make up 80-90% of cases. But about 10-20% of lung cancer patients have never smoked. For them, screening isn’t routinely recommended unless they have other major risk factors like genetic mutations, radon exposure, or a strong family history. Research is ongoing-trials like PACIFIC aim to identify non-smokers who should be screened based on combined risk models.
How effective is targeted therapy for early-stage lung cancer?
For patients with early-stage non-small cell lung cancer and specific mutations like EGFR, targeted therapy like osimertinib has dramatically improved outcomes. The ADAURA trial showed it reduced the risk of cancer returning or spreading by 83% after surgery. This means many patients who once faced high recurrence rates now have a near-normal life expectancy. These therapies work best when cancer is caught early-exactly what screening is designed to do.



Man, this is the kind of post that makes you want to hug your doctor and scream at your insurance company at the same time. I didn’t even know I qualified for screening-I quit smoking 18 years ago, thought I was in the clear. Turns out my 25 pack-years still count. That JAMA Oncology study? Mind blown. We’re talking about a disease that kills more than the whole damn cancer combo platter, and we’re still acting like it’s some secret club you need an invite to join. Time to stop being passive and start being proactive. Your lungs don’t care how ‘reformed’ you are-they just want you to get checked.
Oh please. Another ‘screening saves lives’ PSA. You know what saves lives? Not smoking. Or better yet-stop telling people they need to be scanned like they’re in a dystopian surveillance state. The false positives alone are a nightmare. I know someone who got a biopsy for a ‘suspicious nodule’ that turned out to be a scar from a cold they had in 2012. They lost three weeks of work, $8K, and their sanity. We’re turning medicine into a fear-based industry. And don’t even get me started on AI. Next thing you know, your toaster will diagnose you.
My dad got screened last year. Nodule. Biopsy. Stress. Nothing. He’s 70, smoked 2 packs a day for 30 years. Still, he won’t go back. Says it’s a waste of time. I get it. But he’s alive because he went once. That’s the thing-most people don’t get it until it’s too late.
As a nurse who’s seen too many late-stage cases, I’m screaming this from the rooftops: if you’re eligible, GET SCREENED. Not because someone told you to. Not because it’s ‘recommended.’ But because your life matters more than your fear. And if your doctor doesn’t bring it up? Ask. Politely but firmly. You’re not being annoying-you’re being smart. And if insurance says no? File an appeal. It’s your right. This isn’t optional. It’s survival.
Just got my LDCT scan last week. Zero drama. 10 seconds of holding my breath. Felt like a space alien being scanned. The tech was super chill and explained everything. Got the results back: clear. But honestly? I’m going back next year. Because even if it’s a false alarm, it’s better than being a statistic. Also-huge shoutout to the patient navigator who called me to schedule it. I didn’t even know that was a thing. Why isn’t this standard everywhere?
There’s a critical gap here that nobody talks about: follow-up. Screening is only as good as the system that supports it. I work with a rural clinic in West Virginia. We’ve got the machine. We’ve got the patients. But we don’t have the radiologists who specialize in interpreting nodules. So we send scans to a regional hub. Sometimes it takes 6 weeks. By then, the patient’s anxiety has spiraled, and they’ve stopped showing up. We need infrastructure, not just technology. And we need to pay radiologists fairly to do this work. It’s not glamorous, but it’s life-saving.
Why are we still pretending this is about health? This is capitalism in a lab coat. They want you scared, so you’ll keep coming back for scans, biopsies, and $15,000 pills. Osimertinib costs $20,000 a month. Who’s really benefiting here? Big Pharma. And don’t tell me it’s ‘saving lives’-they’re just selling longer lives at premium prices. Meanwhile, people in India are dying from air pollution and can’t even get a chest X-ray. This isn’t medicine. It’s a luxury subscription.
As a British citizen who’s watched the NHS struggle with cancer care for decades, I find this entire conversation both fascinating and infuriating. In the UK, we don’t have targeted therapies on the NHS unless they pass a cost-effectiveness threshold that often excludes them. We screen, yes-but only for those who meet rigid criteria. And yet, here in the US, you have cutting-edge AI, liquid biopsies, and gene-targeted drugs… but only if you can afford it. The irony? The US leads in innovation but lags in access. Britain leads in equity but lags in innovation. We need both. And we need it now.
My mom died of lung cancer at 59. Never smoked. Never even liked cigarettes. But she lived near a highway for 40 years. Air pollution. Radon in the basement. Family history. No one ever told her to get screened. She had a cough for 8 months. They called it ‘allergies.’ By the time they found it? Stage IV. I hate that no one warned her. I hate that this isn’t common knowledge. I hate that we treat lung cancer like it’s punishment instead of a disease. If you’re reading this? Please. Ask your doctor. Even if you don’t smoke. Even if you think you’re safe. You’re not.
LOL so now we’re gonna screen everyone who ever smoked? What’s next? Mandatory colonoscopies for people who ate a burger in 2003? This is just medical theater. The system’s broken. You get a scan, you get a nodule, you get a biopsy, you get a bill, you get anxiety, you get nothing. And the ‘targeted therapies’? They work for 6 months then the cancer learns to escape. It’s like playing whack-a-mole with your own DNA. Stop selling hope. Start fixing the system.
Here’s the real question: if we can detect cancer before it forms, should we? Liquid biopsies could find tumor DNA years before a nodule appears. But what if we find something we can’t explain? A mutation with no known link? Do we operate? Do we treat? Do we live in fear of a ghost in our blood? Medicine is getting so good at finding things… but we’re not ready to handle the meaning of what we find. We need ethics as much as we need tech.
Let’s be real-96% false positives means we’re doing something wrong. We’re not improving screening; we’re just making more work for radiologists and more trauma for patients. The real solution isn’t more scans-it’s prevention. Tax cigarettes into oblivion. Fund clean air initiatives. Stop letting Big Tobacco lobby Congress. Screening is a Band-Aid on a bullet wound. We’re treating the symptom, not the cause. And until we fix that, we’re just rearranging deck chairs on the Titanic.
My cousin got screened. They found a nodule. She cried for three days. Then she got a second opinion. Then a third. Then she found out the clinic was under-accredited. The radiologist had never seen a lung scan before. She’s now suing. And yes, she’s alive. But this system? It’s a minefield. We need standards. We need accountability. We need to stop letting hospitals cut corners because ‘it’s just a scan.’ It’s not just a scan. It’s someone’s life.
you know what they dont tell you? the government pays for the scan but not the follow up. so if you get a nodule you better have good insurance or good friends with money. also the real reason screening rates are low? people dont trust doctors. after covid and the vax debates and the pharma scandals? why would you believe someone who says 'just lie down for 10 seconds and we'll find your death'?
Wow. So now if you smoked at all in your life, you’re a ticking time bomb? That’s not medicine. That’s guilt-tripping with a CT machine. And who decides what’s ‘high risk’? Some panel in D.C. who’s never held a cigarette? Meanwhile, my neighbor who vapes 300 mg of nicotine a day doesn’t even get a look. Double standard. And don’t get me started on the racial disparities. Black smokers get less screening? No. They get less care. Because the system was built to fail them. This isn’t about screening. It’s about who gets to live.