HIV Prevention Impact Calculator
Program Impact Estimator
This calculator estimates the potential impact of a needle exchange program (NEP) on HIV transmission and healthcare costs in your community.
Estimated Program Impact
New HIV Infections Prevented: 0
HIV Treatment Cost Savings: $0
Program Efficiency Ratio: 0:1
Syringes Distributed Annually: 0
Savings Per Syringe: $0
Program ROI: 0%
Impact Metrics Comparison
| Metric | With NEP | Without NEP | Savings |
|---|---|---|---|
| New HIV infections | 0 | 0 | $0 |
| New Hepatitis C infections | 0 | 0 | $0 |
| Overdose deaths | 0 | 0 | $0 |
| Annual program cost | $0 | - | - |
| Projected treatment savings | $0 | - | - |
Quick Takeaways
- Safe needle exchange programs (NEPs) cut HIV transmission among people who inject drugs by up to 80%.
- Each dollar spent on NEPs saves roughly $4 in HIV treatment costs.
- NEPs also reduce hepatitis C, overdose deaths, and connect users to health services.
- Community opposition often stems from stigma, not data.
- Effective programs need clean syringes, counseling, and strong local partnerships.
What Is a Safe Needle Exchange Program?
When we talk about a safe needle exchange program is a public‑health service that provides sterile syringes to people who inject drugs (PWID) in exchange for used ones, we’re describing a core element of the harm reduction approach that aims to lower health risks without requiring abstinence. The idea is simple: give people clean needles, collect the dirty ones, and use every touchpoint to offer education, testing, and referrals.
Why HIV and AIDS Matter in This Context
The HIV Human Immunodeficiency Virus, the virus that can lead to AIDS spreads easily through shared injection equipment. In the United States, about 10% of new HIV diagnoses each year involve injection drug use. When a syringe is reused, the virus can transfer in a single prick. Over time, this creates pockets of infection that are hard to control without targeted interventions.
AIDS Acquired Immunodeficiency Syndrome, the late stage of HIV infection where the immune system is severely compromised carries a heavy medical and social burden. Preventing the virus from reaching this stage saves lives, reduces hospital stays, and limits the stigma that often follows an AIDS diagnosis.
How NEPs Slash HIV Transmission
Multiple studies-like the 2023 CDC analysis of 42 cities-show that NEPs cut HIV incidence among PWID by 60‑80%. The mechanism is threefold:
- Clean needles stop direct blood‑to‑blood transfer. One fresh syringe eliminates the primary transmission route.
- Every exchange is an opportunity for HIV testing rapid antibody/antigen screening offered on site. Early diagnosis leads to early treatment, which dramatically lowers viral load and future spread.
- Education on safer injection practices and condom use reduces secondary transmission through sexual contact.
Think of an NEP as a tiny triage station on the street-each clean needle is a shield, each test is a radar, each conversation is a map toward treatment.
Cost Savings That Add Up
Health‑care economics paint a clear picture. Treating a new HIV infection over a lifetime can exceed $400,000 in US dollars. A well‑run NEP that distributes 500,000 syringes a year typically costs under $2 million. The World Health Organization WHO, the UN agency that sets global health standards estimates that every dollar spent on needle exchange saves $4-$5 in downstream treatment costs.
Here’s a quick snapshot:
| Metric | With NEP | Without NEP |
|---|---|---|
| New HIV infections | 12 | 58 |
| New Hepatitis C infections | 27 | 73 |
| Overdose deaths | 4 | 9 |
| Annual program cost (USD) | 1.8million | 0 |
| Projected treatment savings (USD) | 7.2million | 0 |
Beyond HIV: Tackling Hepatitis C and Overdose
The same clean‑needle logic applies to Hepatitis C a blood‑borne virus that often co‑occurs with HIV among PWID. Studies in 2024 show a 55% drop in new Hep C cases when NEPs are active.
Many programs also hand out naloxone kits, the antidote for opioid overdose. Communities that added naloxone distribution to their NEPs saw overdose death rates halve within two years.
Community Benefits and Common Misconceptions
Opponents sometimes argue that NEPs enable drug use. The data says otherwise. In cities where NEPs operate, overall drug‑related crime stays flat or declines. People who receive clean needles are more likely to enter treatment programs-up to 30% in some locales-because the program builds trust with health workers.
Another myth is that NEPs increase public litter. Many successful programs include safe disposal bins and partner with local sanitation crews, keeping streets cleaner than before.
Steps to Launch a Successful Program
- Assess Local Need. Gather data from CDC Centers for Disease Control and Prevention, the US public‑health agency and local health departments to quantify PWID populations and infection rates.
- Secure Funding. Apply for federal grants (e.g., HRSA’s Substance Abuse Prevention programs) and seek city budget allocations.
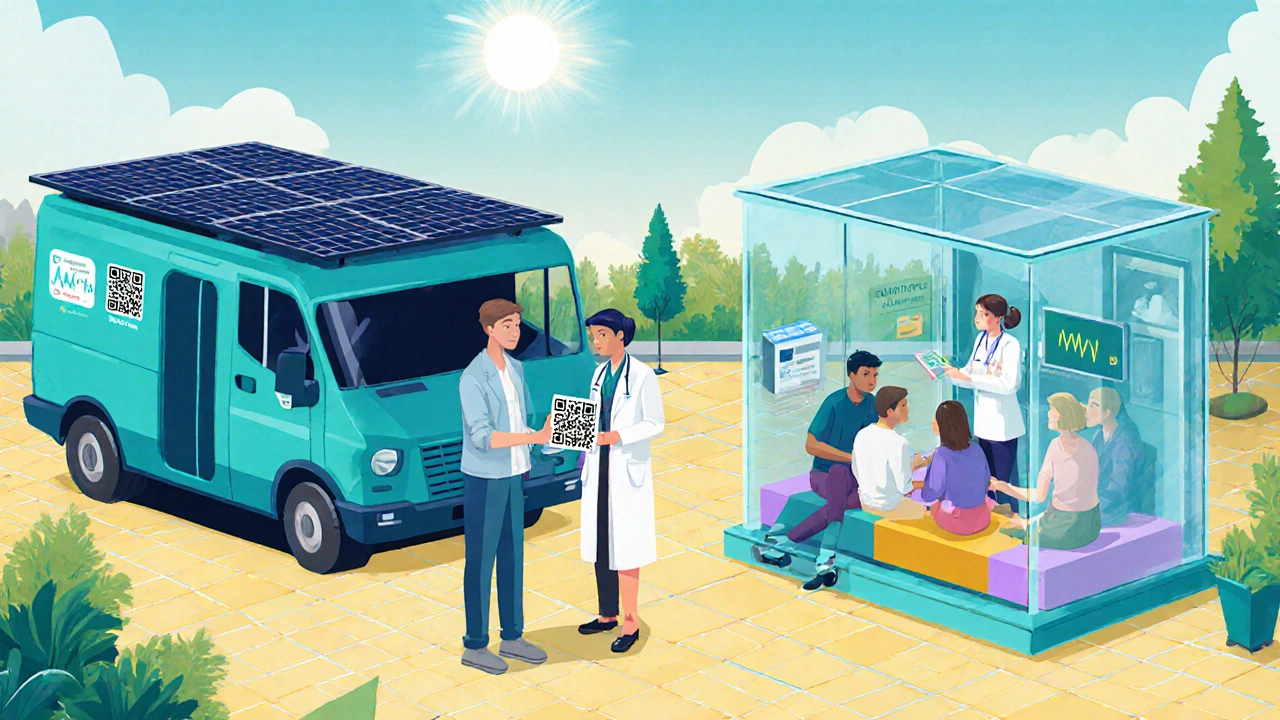
- Choose a Site. Partner with a community health center a local clinic that offers primary care and outreach services or a mobile van that can reach underserved neighborhoods.
- Hire Trained Staff. Recruit nurses, certified peer counselors, and a distributive logistics coordinator.
- Set Up Safe Disposal. Install sharps containers at the site and arrange for regular hazardous‑waste pickup.
- Integrate Services. Offer rapid HIV/Hep C testing, vaccination, counseling, and referrals to medication‑assisted treatment (MAT).
- Monitor and Report. Track distribution numbers, infection rates, and service uptake. Publish quarterly results to maintain transparency.
Following these steps creates a feedback loop: more data leads to better funding, which expands services, which in turn improves health outcomes.
The Future Landscape
Emerging technologies-like QR‑coded syringe packs that link to digital health records-are making it easier to monitor usage while preserving anonymity. Telehealth integration lets program participants schedule virtual visits for PrEP (pre‑exposure prophylaxis) without leaving the site.
Policymakers are also shifting. The 2025 bipartisan health‑security bill includes language that protects funding for NEPs even in states with stricter drug laws. This legislative backbone could standardize safe‑needle access nationwide.
Frequently Asked Questions
Do needle exchange programs increase drug use?
Research consistently shows no increase in drug consumption. Instead, participants are more likely to seek treatment and adopt safer practices.
How many syringes does a typical program provide?
Most urban programs aim for at least 200 syringes per PWID per year, but high‑need areas distribute up to 500 per person.
Can I get HIV testing at a needle exchange?
Yes. Rapid antibody/antigen tests are standard in most NEPs, often delivering results in under 20 minutes.
What happens to the used needles?
Collected syringes go into sealed sharps containers and are incinerated by licensed hazardous‑waste firms, preventing community exposure.
Are there legal risks for participants?
Most jurisdictions grant legal protection for individuals accessing NEPs, but laws vary. It’s best to check local statutes before attending.



Wow, the data on needle exchange programs is absolutely staggering, and anyone who tries to downplay it is clearly ignoring the science 🤦♀️. First, the reduction in HIV transmission rates can be as high as eighty percent, which is a massive public health victory that any sane nation should celebrate. Second, the cost savings are undeniable – every dollar invested returns four to five dollars in avoided treatment expenses, a fact that should make any fiscally‑responsible government sit up straight. Third, let’s not forget the secondary benefits: hepatitis C rates plummet, overdose deaths are cut in half, and countless individuals gain a crucial foothold into treatment and support services. Fourth, the evidence is backed by reputable bodies like the CDC, WHO, and countless peer‑reviewed studies, so the claim that these programs “enable drug use” is a myth peddled by fear‑mongers. Fifth, these programs also provide a humane response to a complex issue, showing compassion instead of casting judgement. Sixth, communities that have embraced NEPs report no uptick in drug‑related crime; in fact, many see a slight decline because the programs often include outreach and counseling that deter risky behavior. Seventh, the safe disposal of used needles protects families and sanitation workers, countering the misguided “litter” argument. Eighth, the integration of rapid HIV testing at these sites means early diagnosis and treatment, which dramatically reduces community spread. Ninth, many programs also distribute naloxone, saving lives by reversing overdoses in the critical minutes before emergency responders arrive. Tenth, the political resistance often stems from stigma rather than data, a sad reminder that ideology still trumps evidence in some policy circles. Eleventh, the implementation steps are clear and replicable, from securing funding to partnering with local health centers, making the barrier to action more about will than logistics. Twelfth, emerging technologies like QR‑coded syringe packs are making data collection easier while preserving anonymity, a win‑win for privacy and public health monitoring. Thirteenth, the recent bipartisan health‑security bill even codifies protections for NEP funding, reinforcing that this is a national priority. Fourteenth, the ripple effect includes reduced healthcare burdens on hospitals, freeing resources for other critical needs. Fifteenth, by reducing the prevalence of HIV and hepatitis C, we improve overall community health and productivity. Sixteenth, let’s be clear: supporting needle exchange is not about condoning drug use, it’s about protecting lives, saving money, and building healthier societies 😤💪.
Oh great another love‑letter to syringes, as if we needed more drama.
I think it’s important to recognize how these programs not only cut infections but also provide a bridge to treatment for many people who might otherwise fall through the cracks. The data showing cost‑effectiveness is compelling, and the community health benefits are clear. Supporting NEPs is a pragmatic step toward a healthier society.
Look, the numbers don’t lie – you can’t argue with hard facts. Yet some folks keep shouting about “moral decay” while ignoring that a single clean needle can prevent a lifelong infection. It’s a simple math problem: dollars spent vs. lives saved. If you’re still stuck on the idea that giving away sterile syringes somehow encourages drug use, you’re just buying into fear‑mongering. The reality is people who use these services are more likely to seek treatment, and that’s a win for everyone. So before you start spouting nonsense, check the research, because the evidence is right there on the page.
From a Canadian perspective, we’ve seen similar successes with needle programs in cities like Vancouver, where the approach has been integrated into broader harm‑reduction strategies. The cultural shift toward viewing drug users as patients rather than criminals has helped reduce stigma and improve public health outcomes. It’s a model worth considering here as well.
Sure, the government wants you to think it’s all benevolent, but every program comes with hidden agendas. They collect data, they monitor movements, they control narratives. It’s all a part of a larger surveillance scheme that pretends to care while probing the community.
Let’s keep the momentum going, folks! The numbers are clear: these programs save lives, cut costs, and build trust in our public health system. By supporting needle exchanges, we’re not just fighting HIV – we’re investing in the wellbeing of our neighborhoods and giving people a real chance at recovery. Keep cheering for evidence‑based solutions and stay positive about the impact we can make together.
Nice points, thanks for the info!
While enthusiasm is appreciated, let’s not overlook the moral obligation to protect the most vulnerable. It’s disheartening to see any justification that places public health goals above human dignity. The statistics should inspire us to act, not to excuse inaction. Compassion must guide policy, not just cold calculations.
One could argue that the very existence of these programs forces us to confront deeper societal questions about addiction, responsibility, and community solidarity. It’s a reminder that health is not merely an individual concern but a collective endeavor, bound by shared humanity.
Ah, the usual spiel about “collective responsibility” while the real power players keep pulling strings behind the curtain. If you think these initiatives are pure altruism, you’re buying into the mainstream narrative that hides the true motives.
🙂 I think it’s great to see the community coming together on this issue. The evidence is solid, and the compassionate approach can only strengthen trust between public health officials and those who need help the most.
Honestly, i think people overhype it, its not a cureall and some folks just keep using cuz they dont want to quit lol.
I totally hear where you’re coming from, and it’s painful to see anyone suffer. The data shows that safe‑needle programs give many a lifeline and a chance to get treatment when they’re ready. It’s a step toward healing, not a judgment.
Exciting times ahead! The integration of tech like QR‑coded packs and telehealth links could make these programs even more effective. Let’s keep pushing for innovation while staying grounded in the core goal: saving lives.
Spot on! The momentum is real, and with solid coaching and aggressive outreach, we can expand these services to reach every community in need.
Esteemed colleagues, I wish to commend the thorough analysis presented herein. The empirical evidence supporting needle exchange programs is robust, and the fiscal prudence delineated aligns with best practices in public health economics. It is incumbent upon policymakers to integrate such evidence‑based interventions promptly.
Great job, thanks for sharing!
While the enthusiastic endorsement of needle exchange programs is understandable, one must scrutinize the broader implications with a critical eye. The data is indeed compelling, yet it is essential to consider potential unintended consequences, such as the risk of normalizing syringe availability without concurrent robust treatment pathways. Moreover, any public health initiative should be evaluated for cost‑effectiveness over the long term, taking into account not only direct healthcare savings but also societal costs related to substance use disorders. The literature points to varied outcomes depending on local implementation fidelity, suggesting that a one‑size‑fits‑all approach may be overly simplistic. Furthermore, the moral discourse surrounding these programs often gets eclipsed by quantitative metrics, yet community values and ethical considerations remain vital components of policy decisions. In sum, while needle exchange programs offer a promising tool in the public health arsenal, they must be deployed within a comprehensive strategy that includes prevention, treatment, and community engagement to truly mitigate the spread of HIV and related harms.
Interesting perspective, thanks for the nuance.