Workplace wellness programs aren’t just about yoga classes and standing desks. The real impact comes from what happens when employees take their pills - or don’t. Nearly half of all Americans don’t take their medications as prescribed. That’s not laziness. It’s often cost. And that’s where pharmacists step in - not as order-takers, but as frontline health strategists.
Why Generics Matter More Than You Think
Generic drugs aren’t cheap knockoffs. They’re the exact same medicine, approved by the FDA, with the same active ingredients, strength, and safety profile as brand-name drugs. The only difference? Price. A 30-day supply of lisinopril (generic for Zestril) might cost $4. A brand-name version? $120. That’s not a typo. For someone managing high blood pressure, that gap can mean skipping doses - or skipping refills entirely. In the U.S., generics make up 90% of all prescriptions filled, but only 22% of total drug spending. That’s a $300 billion annual savings potential. And pharmacists are the ones who turn that potential into reality.The Pharmacist’s Unique Role in Workplace Wellness
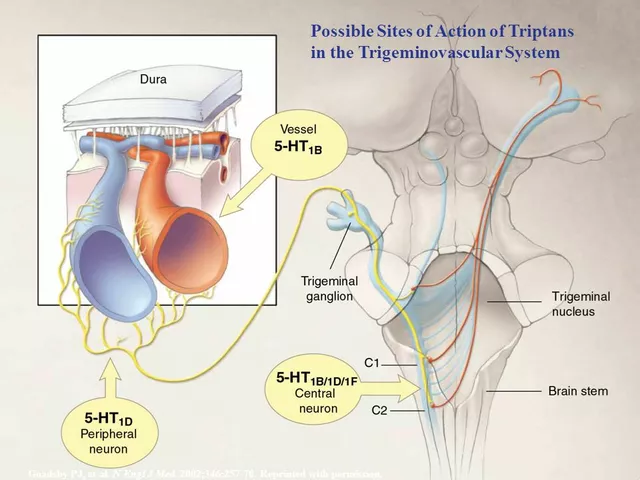
Most wellness programs focus on diet, exercise, or stress. But if an employee can’t afford their diabetes medication, no amount of step challenges will fix their A1C. That’s where pharmacists bring something no other wellness provider can: direct access to medication decisions. In workplace settings, pharmacists are embedded in clinics, telehealth platforms, or partnered with Pharmacy Benefit Managers (PBMs). They don’t just dispense pills. They do Medication Therapy Management (MTM) - a full review of every drug a person takes, checking for duplicates, interactions, and cost-saving opportunities. One study found that when pharmacists lead MTM in workplace programs, medication adherence jumps 15-20%. That’s not a small number. The CDC says better adherence could prevent 125,000 deaths a year in the U.S. alone.How Pharmacists Actually Get People to Switch to Generics
It’s not enough to say, “This is cheaper.” People worry. They think generics are weaker. Slower. Less safe. Pharmacists tackle those fears head-on. They use simple, trusted language: “The ibuprofen you buy at the store is the same as Advil - just without the brand name.” They show patients the FDA’s Orange Book, which lists therapeutically equivalent drugs. They explain bioequivalence: generics must deliver 80-125% of the brand’s absorption rate - meaning they work the same in the body. One pharmacist in Seattle told employees she takes generic metformin herself. “I’m not asking you to take something I wouldn’t,” she said. That personal touch works. Surveys show 78% of employees feel more confident about generics after a pharmacist consultation. They also use tools like McKesson’s OneStop Generics or MAC (Maximum Allowable Cost) lists to find the lowest-cost option that’s still clinically appropriate. If a brand-name drug is the only option covered, they flag it for the prescriber - often leading to a switch.What Employers Are Doing Right
Forward-thinking employers aren’t just offering wellness programs - they’re designing them around medication access. Three-tier formularies are common: generics at the lowest copay, preferred brands higher, non-preferred brands the most expensive. Some companies go further: mandatory generic substitution for chronic conditions like hypertension, diabetes, and high cholesterol. That means if a doctor prescribes a brand-name statin, the pharmacy automatically fills it with the generic unless the doctor says no. Large employers (5,000+ employees) are 68% more likely to include pharmacist-led services in their wellness plans than smaller ones. Why? Because the ROI is clear. For every $1 spent on pharmacist interventions, employers save $7.20 in medical costs. That’s not a guess. It’s from the American Pharmacists Association’s 2024 economic study. Walmart Health Centers, now offering on-site pharmacy services to employer clients, saw a 23% drop in prescription costs among participating employees in just one year. That’s not luck. It’s strategy.The Hurdles Pharmacists Face
It’s not all smooth sailing. State laws vary wildly. In 49 states, pharmacists can substitute generics - but some require prescriber approval for therapeutic interchange. That means if a doctor writes for Lipitor, and the pharmacist wants to switch to atorvastatin, they might need to call the doctor back. That delays care. It defeats the purpose. Some doctors still hesitate to let pharmacists make substitutions, fearing loss of control. But data shows pharmacists correctly identify appropriate substitutions in 98.7% of cases when following FDA and state guidelines. Smaller employers often lack the resources to train pharmacists or integrate them into their systems. Without standardized materials, pharmacists end up making up explanations on the fly. That’s risky. Consistency matters.
What’s Next? The Future Is Clinical
The 2024 PBM Transparency Act is forcing pharmacy benefit managers to stop hiding spread pricing. That means employers will demand more value - and pharmacists are positioned to deliver it. By 2027, the American Pharmacists Association predicts 85% of large employer wellness programs will include pharmacist-led medication optimization. That’s not speculation. It’s the logical next step. Pharmacists are no longer just behind the counter. They’re in the room with HR teams, negotiating benefit designs. They’re on Zoom calls with employees, reviewing med lists. They’re the bridge between clinical care and financial reality. And for employees? It’s simple: they get better health. Lower bills. Fewer hospital visits. All because someone took the time to explain that a $4 pill works just as well as a $120 one.Why This Isn’t Just About Money
It’s easy to reduce this to cost-cutting. But it’s deeper than that. It’s about dignity. About access. About not having to choose between rent and refills. When a pharmacist helps a diabetic employee switch from a $500 brand-name insulin to a $35 generic, they’re not just saving money. They’re giving that person a chance to live. Workplace wellness isn’t about fitness trackers. It’s about whether someone can afford to stay alive. And pharmacists? They’re the ones making sure they can.Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also meet the same strict standards for purity, stability, and performance. Bioequivalence testing ensures they work the same way in the body - within 80-125% of the brand’s absorption rate. Millions of people take generics every day with the same results.
Can pharmacists switch my prescription to a generic without my doctor’s approval?
It depends on your state. In 49 states, pharmacists can substitute a generic for a brand-name drug if it’s listed as therapeutically equivalent in the FDA’s Orange Book. But some states require the prescriber to give permission first - especially for complex conditions like epilepsy or thyroid disorders. Pharmacists follow state law, so if substitution is blocked, they’ll work with your doctor to get approval or find another option.
Why don’t all employers use pharmacists in their wellness programs?
Cost and complexity. Smaller employers often lack the budget or infrastructure to integrate pharmacists directly. They may rely on PBMs that don’t offer clinical services, or they’re unaware of the ROI. But as data grows - showing $7.20 saved for every $1 spent on pharmacist care - more companies are adding these services. The trend is clearly moving toward clinical pharmacist roles in workplace wellness.
What’s the difference between a generic and an authorized generic?
An authorized generic is made by the same company that produces the brand-name drug, just without the brand name on the label. It’s identical in every way - same ingredients, same factory, same packaging (minus branding). These are often cheaper than the brand and sometimes even cheaper than standard generics because they bypass middlemen. Pharmacists often recommend them when available.
How do pharmacists know which generics are safe to substitute?
They use the FDA’s Orange Book, which lists all approved generic drugs and their therapeutic equivalence ratings. A rating of “AB” means the generic is approved as therapeutically equivalent to the brand. Pharmacists also check state laws, formulary rules, and patient history before making any switch. They don’t guess - they follow evidence-based protocols.
Do generics cause more side effects than brand-name drugs?
No. The FDA requires generics to have the same safety profile as the brand. Inactive ingredients (like fillers or dyes) can vary slightly, and in rare cases, someone might have a sensitivity to one of those. But that’s true for brand-name drugs too. If a patient reports a new side effect after switching, the pharmacist investigates - but it’s almost never because the active ingredient changed.

Yeah sure, let’s just trust some guy in a white coat to swap my pills like it’s a game of musical chairs. I’ve seen generics that look like they were made in a basement with a 3D printer. And don’t even get me started on the ‘FDA approved’ nonsense - they approve everything these days. My uncle took a generic for his heart and ended up in the ER. Coincidence? I think not.
ok but like… why are we even talking about this like its some revolutionary idea?? pharmacists have been doing this for DECADES. also the whole ‘$4 vs $120’ thing is so basic its cringe. my mom’s been taking generic metformin since 2012 and she’s still alive?? wild.
Let me just say this - if you think generics are ‘just as good’ you’re either brainwashed by Big Pharma or you’ve never actually read the fine print. I used to work at a pharmacy in Ohio and saw people switch to generics and then come back three weeks later with rashes, dizziness, and panic attacks. The inactive ingredients? Totally different. And yeah, the FDA says ‘bioequivalent’ but that’s just a fancy word for ‘close enough’. What’s close enough for your blood pressure? What’s close enough for your liver? You think they test this stuff on real people or just lab rats? I’m not saying don’t use them - I’m saying don’t be naive. This isn’t science, it’s corporate math dressed up as healthcare.
Generics work fine. Why are you making this so complicated. People in Nigeria take generics daily and live. Your fear is not a fact.
you think america is the only country that cares about health? we in nigeria dont even have insurance but we still take generics and dont die. you americans act like your life is so special but you cant even afford a pill? its not the drug its your system. pharma companies are crooks but you let them be. blame yourselves not the pharmacist.
The 7.20:1 ROI is real. I’ve seen the spreadsheets. But the real win is adherence. No one talks about how much stress this removes from patients. That’s the silent metric.
I work in a rural clinic. Last month, a 68-year-old woman came in crying because she was skipping her insulin doses to pay for her grandson’s school supplies. We switched her to the generic - $35 instead of $500. She cried again. This time from relief. This isn’t about cost-cutting. It’s about dignity. Pharmacists are the only ones who see this side of healthcare - the human side. We need more of them in every workplace, not fewer.
Thank you for this. Seriously. I’ve been trying to tell my HR department for two years that we need pharmacist-led MTM - and now I’ve got the data to back it up. The $7.20 return? That’s not just savings - that’s fewer ER visits, fewer missed days, fewer families breaking apart because someone couldn’t afford their meds. And the part about the Seattle pharmacist taking metformin herself? That’s the kind of trust that changes lives. We’re not just talking about pills - we’re talking about people being able to wake up tomorrow. Let’s stop treating healthcare like a spreadsheet and start treating it like a human right. Pharmacists are the unsung heroes of this whole system. They’re not just filling prescriptions - they’re filling gaps in our society. Let’s give them the platform they deserve.