Every year, thousands of people take evening primrose oil (EPO) for PMS, eczema, or joint pain. But if you’re on antipsychotic medication-or have epilepsy-this common supplement might be riskier than you think. The truth? Experts can’t agree. Some say it’s safe. Others warn it could trigger seizures. And if you’re caught in the middle, you’re left guessing.
What Evening Primrose Oil Actually Does
Evening primrose oil comes from the seeds of a wildflower called Oenothera biennis. It’s packed with omega-6 fatty acids: about 74% linoleic acid and 9% gamma-linolenic acid (GLA). That GLA is the star. Your body turns it into prostaglandin E1, a compound that helps reduce inflammation. That’s why people use it for inflamed skin, painful periods, or arthritis.
But here’s the twist: those same fatty acids interact with brain chemistry in ways that could affect how easily seizures start. In animal studies, EPO components blocked sodium channels-something that usually calms overactive nerve signals. That sounds like it should prevent seizures, right? Yet, doctors still warn against it.
The Seizure Controversy: Two Sides of the Same Coin
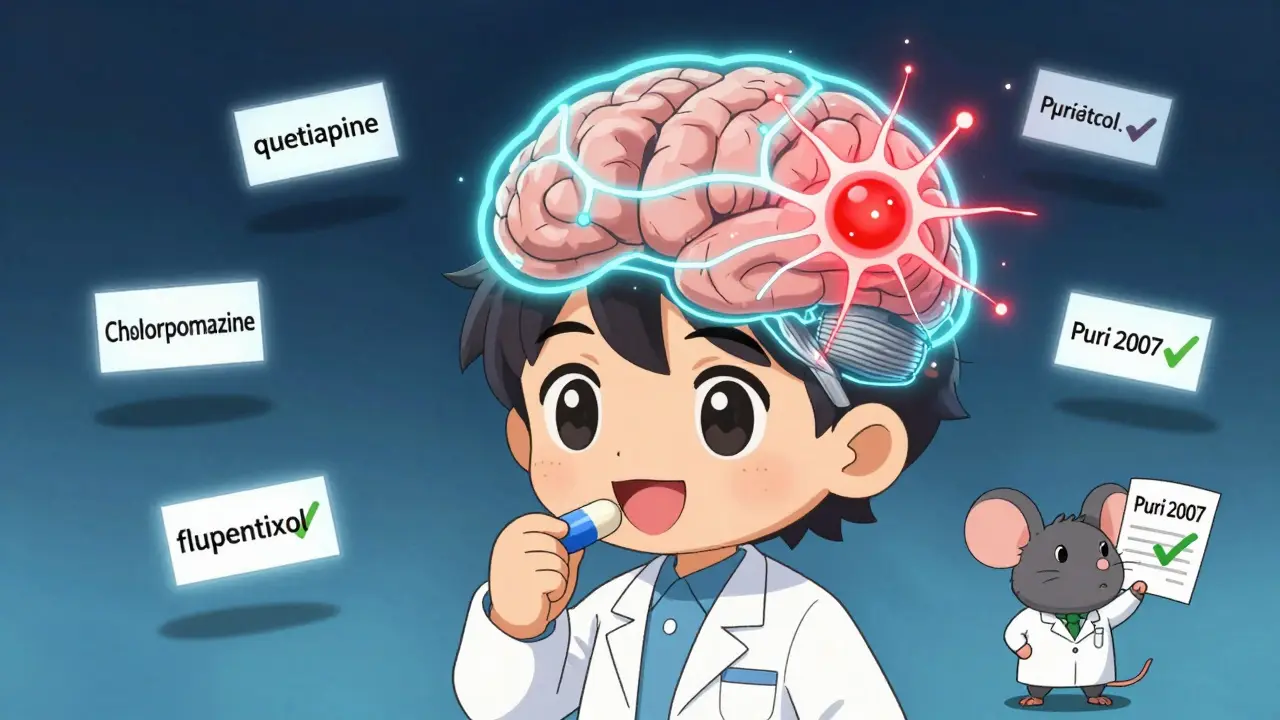
In the early 1980s, a few case reports linked EPO to seizures in people with epilepsy. That was enough for pharmacies and health sites to slap on warnings. But in 2007, Dr. BK Puri from Imperial College London dug deeper. He reviewed decades of data and found no solid proof. In fact, he showed that in four different epilepsy models in rats, EPO actually reduced seizures. His conclusion? The seizure risk is likely a myth.
Yet today, major institutions still say the opposite.
Mayo Clinic’s 2023 guidelines say: Don’t take EPO if you have epilepsy or schizophrenia. Walgreens’ medication guide warns it may interact with antipsychotics and raise seizure risk. Familiprix lists it as a known trigger when combined with drugs like flupentixol (Fluanxol) or chlorpromazine (Largactil). DrugBank adds three more antipsychotics to the list: brexpiprazole, lumateperone, and pimavanserin.
So why the split? One side relies on case reports. The other on controlled studies. One side says ‘play it safe.’ The other says ‘the fear isn’t backed by data.’
How Antipsychotics Fit Into the Picture
Antipsychotics like risperidone, quetiapine, and olanzapine already lower the seizure threshold. That’s why doctors monitor people on these drugs for seizures-even if they don’t have epilepsy. Add EPO into the mix, and the question becomes: does it push things over the edge?
Some data suggests yes. In one documented case, a patient had a seizure under anesthesia after taking EPO. But they were also on multiple other meds. Was it EPO? Or the combo? We don’t know for sure.
Reddit and HealthUnlocked forums show mixed experiences. About 57% of people with epilepsy who took EPO reported no change in seizure frequency. But 32% said their seizures got worse-especially when they added EPO to quetiapine. That’s not a huge number, but it’s enough to make neurologists pause.
And here’s the kicker: the Epilepsy Foundation says the risk is theoretical. But they still advise caution. Why? Because even one bad outcome matters when you’re talking about brain activity.
What the Science Actually Says About Risk
The American Academy of Neurology rated the evidence linking EPO to seizures as Class IV-the lowest level. That means: no large, well-designed human trials. Just case reports, animal studies, and biological plausibility.
That’s not nothing. But it’s not proof either.
DrugBank confirms one clear interaction: EPO increases seizure risk when taken with amifampridine. That’s a rare drug used for Lambert-Eaton syndrome. For most antipsychotics? The link is murky.
Meanwhile, Puri’s 2007 paper-cited 36 times-shows GLA might help protect against seizures. His work suggests the brain’s response to EPO is more complex than a simple ‘lowers threshold’ label.
So what’s the real risk? It’s not zero. But it’s also not proven.
What You Should Do Right Now
If you’re taking antipsychotics or have epilepsy, here’s what matters:
- Don’t stop your meds. Never quit antipsychotics or seizure drugs without talking to your doctor.
- Don’t start EPO without asking. Tell your neurologist or psychiatrist you’re thinking about it. Bring up the conflicting advice. Ask if your specific meds have known interactions.
- Check the label. Most EPO bottles now say ‘avoid if you have epilepsy.’ That’s not just a legal disclaimer-it’s a signal that someone, somewhere, had a bad experience.
- Watch for changes. If you’ve been taking EPO and notice more frequent seizures, confusion, or unusual muscle twitching, stop it and call your doctor immediately.
There’s no universal answer. For some, EPO helps with painful periods without a single seizure. For others, even a 500mg capsule triggers a change. It depends on your brain, your meds, your genetics, and your dose.
The Bigger Picture: Why This Keeps Happening
The global EPO market hit $187.5 million in 2023. Sales are growing. And 22% of epilepsy patients use supplements. That’s a lot of people mixing natural remedies with powerful drugs.
Supplement labels aren’t regulated like prescription drugs. A bottle labeled ‘500mg’ might have 450mg or 550mg. Some brands add fillers. Others don’t test for purity. You can’t assume consistency.
And here’s the sad part: most people don’t tell their doctors about supplements. They think, ‘It’s natural, so it’s safe.’ But natural doesn’t mean harmless. St. John’s wort interferes with antidepressants. Vitamin K messes with blood thinners. And EPO? It might mess with your brain’s electrical balance.

What’s Coming Next
A major study is underway. Launched in January 2024, it’s tracking 300 epilepsy patients over 18 months to see if EPO really affects seizure frequency. The NIH is funding it with $2.3 million. Results won’t come until 2026.
Until then, the European Medicines Agency says: Current evidence doesn’t prove EPO causes seizures-but we need more research on drug combinations.
That’s the middle ground. No panic. No green light. Just waiting for better data.
Alternatives to Evening Primrose Oil
If you’re taking antipsychotics and want to manage PMS, eczema, or inflammation, here are safer options:
- Flaxseed oil or chia seeds for omega-3s-less risk of neurological interactions.
- Topical moisturizers with ceramides or colloidal oatmeal for eczema.
- Calcium and magnesium supplements for PMS cramps-both are well-studied and safe with antipsychotics.
- Curcumin (turmeric extract) for inflammation, if you’re not on blood thinners.
None of these have the same controversy around seizure risk. And they’re easier to track with your doctor.
Final Thought: Trust Your Body, But Verify With Your Doctor
There’s no perfect answer. Some people take EPO for years without issue. Others have a seizure after one dose. The science is split. The market is booming. The warnings are everywhere.
But your health isn’t a statistic. It’s your brain, your nerves, your daily life.
If you’re on antipsychotics or have epilepsy, the safest move isn’t to guess. It’s to ask. Show your doctor your supplement bottle. Ask: ‘Is this safe with my meds?’ Don’t assume it’s fine because it’s natural. Don’t assume it’s dangerous because it’s on a warning label.
Wait for the 2026 study. But until then, don’t take risks with your brain’s stability.
Can evening primrose oil cause seizures in people taking antipsychotics?
There’s no definitive proof, but the risk is real enough that major health institutions warn against it. Case reports link EPO to seizures in people on antipsychotics like quetiapine, chlorpromazine, and flupentixol. While some studies suggest EPO may actually protect against seizures, others show it can lower the seizure threshold-especially when combined with certain drugs. Until more data is available, it’s safest to avoid EPO if you’re on antipsychotics or have epilepsy.
Is evening primrose oil safe for people with epilepsy?
Major organizations like Mayo Clinic and the Epilepsy Foundation say no. They cite case reports and theoretical risks. But a 2007 review by Dr. BK Puri found no clinical evidence that EPO causes seizures-and even suggested it might help prevent them. The contradiction remains unresolved. If you have epilepsy, talk to your neurologist before taking EPO. Never start or stop based on online advice alone.
Which antipsychotics interact most with evening primrose oil?
Familiprix and DrugBank specifically flag flupentixol (Fluanxol), chlorpromazine (Largactil), and amifampridine as high-risk combinations. More recently, brexpiprazole, lumateperone, and pimavanserin were added to the list. These drugs already lower the seizure threshold, and adding EPO may increase that risk. If you’re on any of these, avoid EPO unless your doctor approves it after reviewing your full medication history.
How much evening primrose oil is considered risky?
There’s no set dose that’s ‘safe’ or ‘dangerous.’ Most supplements contain 500mg to 1,300mg per capsule. Higher doses mean more GLA, which could increase biological effects. But risk isn’t just about dose-it’s about your brain chemistry, other meds, and individual sensitivity. Even a single 500mg capsule has triggered seizures in rare cases. The safest approach is to avoid it entirely if you’re at risk.
Are there safer supplements for PMS or eczema if I’m on antipsychotics?
Yes. For PMS, calcium and magnesium supplements are well-studied and safe with antipsychotics. For eczema, topical ceramide creams or colloidal oatmeal baths are effective and carry no neurological risk. Flaxseed oil provides omega-3s without the seizure concerns linked to EPO. Always check with your doctor before starting any new supplement, even if it’s labeled ‘natural’ or ‘gentle.’