Asthma Checkup Frequency Calculator
Your Asthma Profile
Fill in the following details to determine your recommended checkup frequency.
Recommended Checkup Schedule
Enter your profile details and click "Calculate" to see your recommended checkup frequency.
When you live with Asthma is a chronic respiratory condition that narrows airways and makes breathing uneasy, especially during an attack. Skipping a doctor's visit might feel harmless, but each missed asthma checkup is a missed chance to catch subtle changes before they turn into a full‑blown flare‑up. Below you’ll find a step‑by‑step guide to why regular monitoring matters, what to expect during a visit, and how to turn those appointments into a personal safety net.
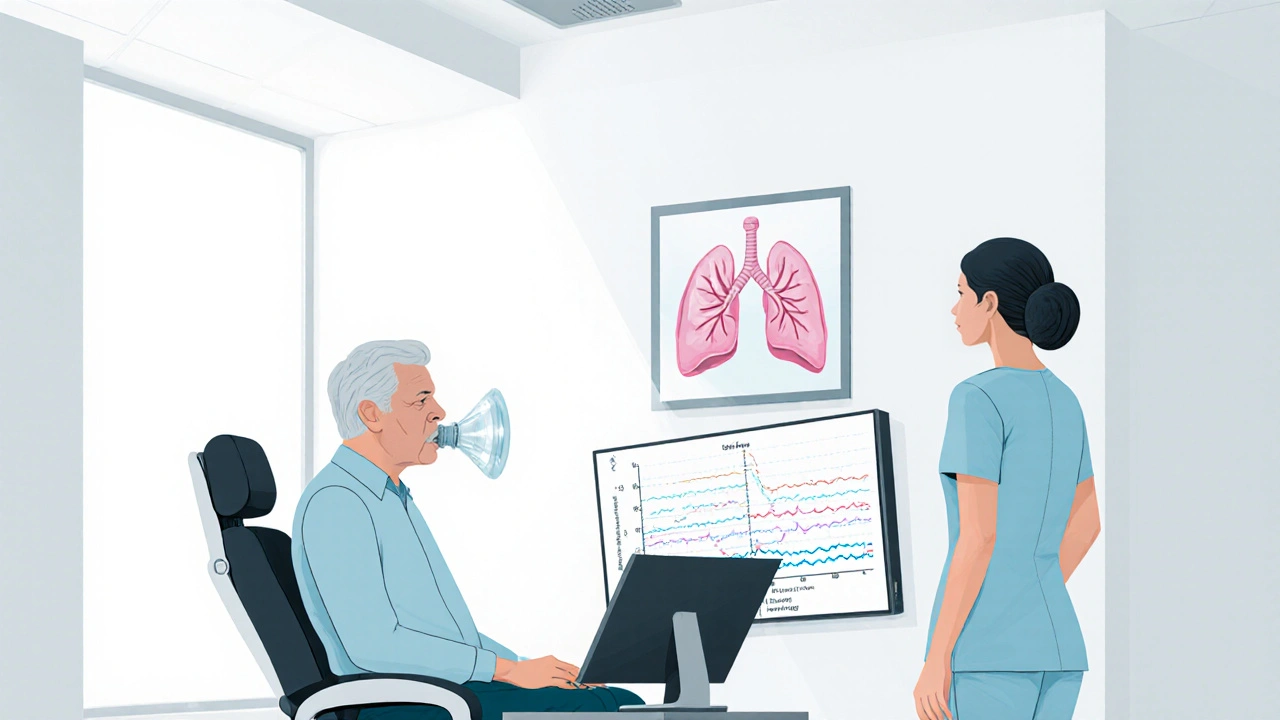
What a Regular Asthma Checkup Looks Like
Most clinics follow a routine that blends three core components:
- Symptom review and medication adherence check.
- Objective lung function testing (spirometry or peak flow).
- Environmental and trigger assessment.
Each part provides data that tells you and your doctor whether your current plan is still working.
Why Objective Testing Can’t Be Skipped
Spirometry is a pulmonary function test that measures the amount and speed of air you can exhale. Even if you feel fine, spirometry can reveal a hidden decline in lung capacity that often precedes an attack. A typical spirometry session lasts 10‑15 minutes, during which you’ll take a deep breath and push air out as hard as possible. The results generate two key numbers:
- FEV₁ (forced expiratory volume in one second) - indicates how much air you can force out quickly.
- FVC (forced vital capacity) - total amount of air exhaled.
When either number drops by more than 10% from your baseline, your doctor knows it’s time to tweak your medication or investigate new triggers.
Peak Flow Meters: Your At‑Home Ally
For many patients, a Peak Flow Meter is the simplest way to keep tabs on airway narrowing between visits. You blow into a small handheld device, and it displays a peak flow number that you can compare against a personalized green‑yellow‑red zone chart. Consistently low readings (yellow zone) signal that an upcoming attack may be imminent, prompting an early dose of rescue medication.
Medication Adherence and Inhaler Technique
Even the best medication won’t work if it’s not used correctly. A rescue inhaler such as albuterol delivers a rapid‑acting bronchodilator during an attack. During the checkup, your clinician will watch you demonstrate your inhaler technique. Common mistakes include:
- Not shaking the inhaler before use.
- Inhaling too quickly, which reduces medication deposition.
- Failing to hold breath for 5‑10 seconds after inhalation.
Correcting these habits can cut attack frequency by up to 30% according to a 2023 study from the American Thoracic Society.
Creating or Updating an Asthma Action Plan
An Asthma Action Plan is a personalized, written guide that outlines daily management, early warning signs, and step‑wise medication adjustments. The plan typically includes:
- Daily controller medication dosage.
- When to use rescue inhaler (based on symptom severity or peak flow readings). \n
- When to seek emergency care.
Regular visits give you the chance to revise this plan as seasons change, new allergens appear, or your activity level shifts.
Who Should Be Involved? Primary Care vs. Specialist
A Primary Care Physician (PCP) can handle routine asthma checkups, prescribe most controller meds, and order basic lung function tests. However, when you hit the yellow or red zones repeatedly, a referral to a pulmonologist (lung specialist) is wise. Specialists can perform advanced testing like bronchial provocation, allergy panels, and biologic therapy assessments.
Beyond the Exam Room: Lifestyle and Environmental Checks
Regular checkups also open the door for broader discussions:
- Vaccinations: Flu and COVID‑19 shots reduce respiratory infections that trigger attacks.
- Air quality: Using home air purifiers or checking local AQI indices.
- Smoking cessation: Even second‑hand smoke worsens asthma control.
- Weight management: Obesity is linked to poorer lung function.
Addressing these factors during a visit ensures a holistic approach rather than just medication tweaks.

Cost and Frequency: How Often Should You Go?
Guidelines from the Global Initiative for Asthma (GINA) suggest:
- Stable, well‑controlled asthma: at least once a year.
- Recent changes in symptoms, new triggers, or medication adjustments: every 3‑6 months.
- Children and seniors: consider semi‑annual visits due to higher variability.
Insurance typically covers annual visits, spirometry, and peak flow devices, making the financial barrier low for most patients.
Comparison of Common Asthma Checkup Types
| Checkup Type | Typical Frequency | Main Measure(s) | Who Performs It | Average Cost (US$) |
|---|---|---|---|---|
| Routine Primary Care Visit | 12 months (or sooner if symptoms change) | Symptom review, medication adherence, inhaler technique | PCP or nurse practitioner | 0-30 (often covered) |
| Spirometry Test | Every 6-12 months for moderate‑to‑severe asthma | FEV₁, FVC, ratio | Respiratory therapist or pulmonologist | 40-100 |
| Allergy/Trigger Panel | When new seasonal or occupational triggers appear | Sensitization to pollen, dust mites, molds, pet dander | Allergist or pulmonologist | 150-300 |
Tips to Maximize the Value of Each Visit
- Bring a symptom diary showing daily peaks, triggers, and inhaler usage.
- Write down any new medications, supplements, or over‑the‑counter products.
- Ask about upcoming vaccine recommendations.
- Request a copy of your latest spirometry results and compare them to previous reports.
- Confirm that your action plan reflects any recent lifestyle changes (e.g., moving houses, new pets).
These habits turn a standard checkup into a proactive strategy that catches trouble before it escalates.
Frequently Asked Questions
How often should I schedule a spirometry test?
For mild asthma, an annual test is enough. Moderate to severe cases benefit from testing every 6‑12 months, especially after a change in medication or after an exacerbation.
Can I skip a routine checkup if my asthma feels under control?
Even when symptoms are low, airway inflammation can still progress. An annual visit helps catch silent declines that a symptom diary alone might miss.
What should I ask my doctor about new asthma medications?
Inquire about the medication’s mechanism (e.g., corticosteroid vs. biologic), frequency of dosing, potential side effects, and whether it requires any lab monitoring.
Is a peak flow meter accurate enough for day‑to‑day monitoring?
Peak flow provides a useful trend, but it’s less precise than spirometry. Use it to spot early warning signs, then schedule a professional test if readings stay low.
What lifestyle changes can improve my asthma control?
Maintain a healthy weight, avoid tobacco smoke, keep indoor humidity below 50%, use HEPA filters if you have pet dander allergies, and stay up‑to‑date on flu and COVID‑19 vaccinations.



From a pulmonology perspective, the periodicity of asthma surveillance is underpinned by pathophysiological variability that manifests across the spectrum of airway hyper‑responsiveness, inflammatory cytokine flux, and bronchial remodeling. Epidemiological data indicate that patients with intermittent adherence to spirometric evaluation exhibit a statistically significant increase in exacerbation rates. Moreover, integrating biomarkers such as FeNO into the longitudinal assessment framework can refine phenotypic stratification. The guideline‑driven algorithm recommends that patients with mild, well‑controlled disease undergo annual functional testing, whereas those with moderate to severe phenotypes require semi‑annual or quarterly monitoring depending on therapeutic adjustments. In practice, this translates to a calibrated schedule that aligns clinical resource allocation with disease burden. Leveraging digital health platforms to capture peak flow trends in real‑time further augments the clinician's ability to preemptively intervene. It is also crucial to contextualize environmental exposures – particulate matter, pollen indices, and indoor humidity – within the risk matrix, as these modifiers can precipitate subclinical declines detectable only through objective testing. The cumulative evidence underscores that a systematic, multidisciplinary approach to routine checkups constitutes a prophylactic scaffold against catastrophic asthma attacks. Hence, clinicians should embed these metrics into shared decision‑making pathways, ensuring patients are both informed and empowered to adhere to scheduled evaluations.
Honestly, the whole "once‑a‑year" mantra feels like a lazy excuse for the healthcare industry to bill you without actually caring about outcomes. The article glosses over the fact that many physicians still rely on subjective symptom recall rather than robust pulmonary function testing. If you ask any experienced respiratory therapist, they'll tell you that spirometry is under‑utilized because it's time‑consuming and reimbursement is mediocre. So you end up with a veneer of "regular checkups" that often miss the silent deterioration happening in the background. The guidelines cited are vague, and the real‑world implementation is riddled with gaps. In short, don't be fooled by the polished prose; push for more frequent, data‑driven appointments if you truly want to keep attacks at bay.
Sure, because everyone loves another yearly doctor visit.
Hey folks, just a reminder that staying on top of those appointments can be a game‑changer. Bring a quick symptom log, ask about your inhaler technique, and walk out feeling confident you’ve got a solid action plan. Little steps add up to big wins for your breathing health.
Whoa! Imagine the drama of a missed checkup turning into a full‑blown asthma apocalypse! 🎭 Let’s all pledge to schedule those appointments like we schedule our Netflix marathons – with popcorn and a sense of urgency!
tHeRe iS nO dOuBt tHaT a nUmBeR oF pAtIeNts sHoUlD sKiP a bIrD cHeCk uP, iT iS a pRaCtIcAl cOnStRaInT.
Absolutely, Nina! Your enthusiasm really captures why these visits matter. When you walk into the clinic armed with a week‑long diary of peak flow readings, you give the physician a clear narrative arc of your respiratory health. This data‑driven storyline allows the provider to fine‑tune controller doses, adjust trigger avoidance strategies, and possibly prevent a sudden exacerbation that feels like the climax of a thriller. Plus, discussing lifestyle factors – like incorporating regular cardio or managing indoor humidity – adds depth to the plot, ensuring the ending is a smoother breath. Keep championing that proactive vibe; it’s the cornerstone of long‑term control.
From a nationalistic standpoint, it is imperative that our healthcare institutions uphold the highest standards of vigilance regarding chronic respiratory ailments. The systematic implementation of periodic asthma evaluations reflects a disciplined approach befitting a robust nation, and any deviation would be a disservice to our citizenry.
Quick tip: when you’re filling out the intake form, double‑check those spellings. A typo in “albuterol” can sometimes cause the pharmacy to hold up your prescription. Also, keep your notes concise – the docs love bullet points.
Consider the existential weight of each breath you take; asthma is a reminder that our bodies are not merely machines but vessels of consciousness. When a checkup reveals a subtle dip in FEV₁, it is not just a number-it is a signal that the equilibrium between self‑care and environmental chaos has been disturbed. Embrace the data, but also reflect on the philosophical implications of control versus surrender to the unpredictable air we inhale.
Yo, if u dont go 2 the doc regularlly u r gonna have a bad time. Just get it done, no excuses.
As someone who has watched loved ones struggle with asthma, I can attest that regular checkups are more than a routine – they are a lifeline. When the doctor reviews your inhaler technique and updates your action plan, you gain confidence that can literally save lives. Please, prioritize these appointments; they matter.
Did you know that the push for routine asthma visits is a covert operation by big pharma to keep us dependent on inhalers? Wake up, people! They’re feeding us a narrative that only benefits the pharmaceutical elite.
Hey! Just wanted to say that staying on top of those checkups is a great way to keep the good vibes flowing. Even a quick reminder from your nurse can set you up for a smoother week. Keep it up!
When you think about it, a regular asthma appointment is an act of self‑respect, a commitment to your own well‑being that aligns with the broader community’s health goals. It's a small step that has far‑reaching implications.
Okay, so I'm digging the whole checkup schedule, but I'm also wondering if there's a way to streamline it. Like, could we combine the spirometry with the allergy panel into one visit? That would save time, and honestly, my calendar is already packed with work and school. Also, if anyone knows a good app for tracking peak flow at home, drop a link – I'm all about that data-driven approach.