Antidepressant Selection Guide
Which Antidepressant Is Right for You?
Answer a few questions about your symptoms, medical history, and preferences to see which antidepressants might be most suitable for your situation.
Recommended Options
Choosing an antidepressant can feel like navigating a maze of brand names, side‑effect profiles, and insurance formularies. Paroxetine is a popular SSRI, but it’s not the only player on the field. This guide breaks down how Paroxetine stacks up against its most common alternatives, helping you weigh efficacy, tolerability, cost, and drug‑interaction risk in plain language.
What Is Paroxetine?
Paroxetine is a selective serotonin reuptake inhibitor (SSRI) approved for major depressive disorder, generalized anxiety disorder, obsessive‑compulsive disorder, panic disorder, and post‑traumatic stress disorder. It was first marketed in the early 1990s and quickly became a go‑to option because it works at relatively low doses and is available in both immediate‑release and controlled‑release formulations.
Mechanistically, Paroxetine blocks the serotonin transporter (SERT), increasing serotonin levels in the synaptic cleft. Higher serotonin improves mood and reduces anxiety for many patients, typically after 4-6 weeks of consistent dosing.
How Does Paroxetine Compare to Other SSRIs?
SSRIs share the same basic mechanism, but they differ in half‑life, side‑effect spectrum, and drug‑interaction potential. Below is a quick snapshot of the three most prescribed SSRIs alongside Paroxetine.
| Drug | Typical Daily Dose | Half‑Life | Common Side Effects | Drug‑Interaction Risk |
|---|---|---|---|---|
| Paroxetine | 20‑60 mg | ≈21 h | Nausea, sexual dysfunction, weight gain | High (CYP2D6 inhibition) |
| Sertraline | 50‑200 mg | ≈26 h | Diarrhea, insomnia, sexual dysfunction | Moderate |
| Escitalopram | 10‑20 mg | ≈27‑32 h | Dry mouth, nausea, sexual dysfunction | Low to moderate |
| Fluoxetine | 20‑60 mg | 2‑4 days (active metabolite 7‑15 days) | Insomnia, agitation, sexual dysfunction | Low (CYP2D6 inducer) |
Beyond SSRIs: When an SNRI Might Be a Better Fit
If serotonin‑only modulation doesn’t give you relief, doctors often look to serotonin‑norepinephrine reuptake inhibitors (SNRIs). The two most common SNRIs are Venlafaxine and Duloxetine. They block both serotonin and norepinephrine reuptake, which can help patients with severe depression or chronic pain.
Key differences:
- Venlafaxine often starts at 75 mg/day and can be titrated up to 375 mg. It has a shorter half‑life (≈5 h) and may cause withdrawal symptoms if stopped abruptly.
- Duloxetine is usually dosed at 30‑60 mg daily. It also treats neuropathic pain and fibromyalgia, making it a two‑in‑one choice for some patients.
How to Choose the Right Medication for Your Situation
Consider these six practical factors when weighing Paroxetine against its alternatives:
- Medical History - If you have a history of heart rhythm issues, avoid Fluoxetine (which can affect QT interval) and consider Paroxetine’s moderate cardiovascular profile.
- Sexual Side Effects - All SSRIs can impair libido, but Paroxetine and Sertraline tend to rank highest for this problem. Escitalopram may be a gentler option.
- Drug Interactions - Paroxetine is a strong CYP2D6 inhibitor, so it can raise levels of many other drugs (e.g., certain beta‑blockers, antipsychotics). If you’re on polypharmacy, an SNRI with fewer interactions might be safer.
- Withdrawal Risk - Short‑half‑life agents like Paroxetine and Venlafaxine need a taper schedule. Long‑acting Fluoxetine often works as a “bridge” for patients who fear withdrawal.
- Cost & Insurance - Generic Paroxetine and Sertraline are usually under $10/month, while newer SNRIs can cost $30‑$50 unless covered by a formulary.
- Specific Symptoms - If anxiety is the primary complaint, Paroxetine’s FDA‑approved label includes panic disorder and PTSD. If you need pain relief, Duloxetine’s dual‑action can be decisive.
Side‑Effect Snapshot: What to Expect
Below is a concise overview of the most common side effects for each drug. Frequencies are based on FDA prescribing information and large‑scale meta‑analyses up to 2024.
| Drug | Nausea | Insomnia | Weight Change | Sexual Dysfunction |
|---|---|---|---|---|
| Paroxetine | 30‑40% | 15‑25% | Weight gain 5‑10 lb (common) | 45‑55% |
| Sertraline | 20‑30% | 10‑20% | Weight neutral to slight gain | 35‑45% |
| Escitalopram | 15‑25% | 10‑15% | Weight neutral | 30‑40% |
| Fluoxetine | 18‑28% | 5‑10% (often insomnia) | Weight loss or neutral | 25‑35% |
| Venlafaxine | 22‑32% | 12‑22% | Weight neutral | 30‑40% |
| Duloxetine | 20‑30% | 8‑15% | Weight neutral | 25‑35% |

Real‑World Scenarios: Who Ends Up on Which Drug?
Case 1 - Young adult with anxiety: A 26‑year‑old college student reports panic attacks and social anxiety. After a thorough screen, the clinician chooses Paroxetine because of its strong evidence for panic disorder and the patient’s insurance covers the generic form.
Case 2 - Middle‑aged professional with chronic pain: A 48‑year‑old accountant suffers from major depressive disorder and fibromyalgia. The doctor prescribes Duloxetine to hit both mood and pain pathways, avoiding the sexual side‑effects that the patient worries about.
Case 3 - Senior on multiple meds: A 72‑year‑old managing hypertension, type‑2 diabetes, and depression. Because Paroxetine strongly inhibits CYP2D6, the clinician picks Escitalopram to minimize interaction risk.
How to Switch Safely
Never stop an antidepressant abruptly. A typical taper schedule for Paroxetine looks like this:
- Week 1‑2: Reduce dose by 10 mg (or 25% of the current dose).
- Week 3‑4: Cut another 10 mg.
- Week 5‑6: Switch to the new medication at a low starter dose.
Always coordinate with your prescriber; they may add a short bridge of a long‑acting SSRI such as Fluoxetine to soften withdrawal.
Bottom Line: When Paroxetine Makes Sense
Paroxetine shines for patients who need a solid, FDA‑approved option for anxiety‑heavy disorders, have affordable generic coverage, and can tolerate its modest weight‑gain tendency. If you’re worried about sexual side effects, drug interactions, or withdrawal, look to Escitalopram, Sertraline, or an SNRI instead.
Is Paroxetine safe for long‑term use?
Clinical guidelines consider Paroxetine safe for years of continuous therapy, provided you have regular check‑ups for weight, sexual function, and any emerging side effects. Some doctors prefer to rotate to a different SSRI after a few years to reduce tolerance, but evidence doesn’t show a hard safety ceiling.
How quickly does Paroxetine start working?
Most patients notice mood improvement after 2-4 weeks, but the full therapeutic effect often emerges around week 6. It’s normal to feel a bit more anxious during the first two weeks as serotonin levels adjust.
Can I take Paroxetine with other antidepressants?
Combining two serotonergic drugs raises the risk of serotonin syndrome-a potentially serious condition. Only a psychiatrist should manage such combos, typically using very low doses and close monitoring.
What should I do if I miss a dose?
Take the missed pill as soon as you remember, unless it’s almost time for your next dose. In that case, skip the missed one-don’t double up, as this can increase side‑effects.
Is Paroxetine safe during pregnancy?
Paroxetine carries a known risk of cardiac malformations when taken in the first trimester. Most obstetricians opt for safer alternatives like Sertraline if an antidepressant is needed during pregnancy.


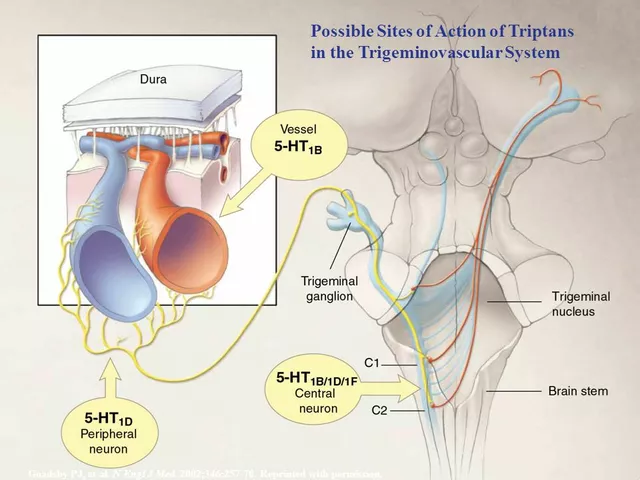
Paroxetine’s CYP2D6 inhibition is not just a footnote; it fundamentally reshapes the metabolic landscape for any concomitant medication. When you add a beta‑blocker that relies on CYP2D6 clearance, you can end up with plasma concentrations that are twice what the label predicts. The weight‑gain profile, often dismissed as “minor,” can be clinically significant for patients already battling metabolic syndrome. Moreover, the sexual dysfunction rates hover around 50 %, eclipsing many of its SSRI peers. If you’re on a statin or an anticoagulant, the interaction potential escalates dramatically-something most clinicians glance over. Bottom line: Paroxetine demands a meticulous medication reconciliation every single visit.
When navigating the therapeutic labyrinth of antidepressants, it is essential to adopt a holistic framework that accounts for pharmacodynamic nuances, patient‑specific variables, and systemic factors such as insurance formularies. Paroxetine, while historically celebrated for its potency in anxiety‑dominant presentations, carries a pharmacokinetic profile that necessitates vigilant monitoring. Its relatively short half‑life of approximately twenty‑one hours predisposes patients to discontinuation syndrome if tapering is not meticulously structured, a consideration that cannot be overemphasized in clinical practice. In contrast, agents such as fluoxetine, with an active metabolite persisting for up to two weeks, may serve as a strategic bridge during transitions, thereby mitigating withdrawal phenomena. Moreover, the drug’s strong CYP2D6 inhibition may precipitate elevated plasma concentrations of concomitant medications ranging from antipsychotics to certain antiarrhythmics, compelling prescribers to either adjust dosages or select alternative agents with a more benign interaction profile. Cost considerations also merit attention; generic paroxetine frequently falls below ten dollars per month, rendering it accessible for patients whose insurance mandates high‑deductible plans. However, affordability must be weighed against the potential for adverse effects that could impair adherence, especially sexual dysfunction, which afflicts nearly half of recipients and often leads to premature discontinuation. For patients with comorbid chronic pain, serotonin‑norepinephrine reuptake inhibitors such as duloxetine may offer a dual‑benefit strategy, addressing both mood and nociceptive pathways. The therapeutic decision matrix should further incorporate the patient’s age, as geriatric populations exhibit heightened sensitivity to anticholinergic load and orthostatic hypotension, risks that are amplified by paroxetine’s anticholinergic properties. In pregnant patients, the teratogenic signal associated with first‑trimester exposure to paroxetine underscores the necessity of alternative selection, typically favoring sertraline based on current obstetric guidelines. Behavioral interventions, including cognitive‑behavioral therapy, remain indispensable adjuncts, as they can reduce the required pharmacologic dose and consequently diminish side‑effect burden. Clinicians must also educate patients about the expected latency of clinical improvement, emphasizing that while some symptomatic relief may become noticeable within two to four weeks, the full therapeutic effect often materializes only after six weeks of consistent dosing. Finally, it is prudent to schedule regular follow‑up assessments at four‑week intervals initially, allowing for dose titration, side‑effect management, and reinforcement of adherence strategies. By integrating these multidimensional considerations, practitioners can tailor antidepressant therapy to the individual’s unique clinical portrait, optimizing outcomes while minimizing iatrogenic complications.
Look, most people think all SSRIs are interchangeable, but paroxetine is a nightmare for anyone who values a stable daily routine. Its short half‑life turns a missed dose into a mini‑withdrawal that can leave you jittery for days. If you’re already juggling work and family, that kind of roller‑coaster is overkill. And don’t get me started on the weight gain-few drugs mess with your waistline like this one. Bottom line, unless your psychiatrist is a fan of constant dose adjustments, you’re better off with sertraline or escitalopram.
Enough of the doom‑and‑gloom attitude, Ben. If you’re truly committed to getting better, you can handle the schedule and the side‑effects-just follow a strict taper plan and keep a symptom diary. Push through the initial jittery phase and you’ll see the mood lift you’re looking for. No excuses, just disciplined adherence.
In the grand tapestry of neurochemical orchestration, paroxetine serves as a modest thread weaving through the synaptic loom, yet its impact reverberates like a quiet echo across the psyche. The paradox lies in its capacity to both liberate and imprison, granting serotonin’s sweet release while shackling the metabolism of countless companions. It is a reminder that every pharmacologic choice whispers a deeper truth about our desire to control the ungovernable currents of the mind.
From a pharmacokinetic standpoint, paroxetine’s high affinity for the serotonin transporter renders it a first‑line SERT inhibitor despite its pronounced CYP2D6 inhibition profile.
The shadows of doubt creep in whenever a pill named paroxetine is mentioned its presence alone can summon a storm of insomnia and weight that gnaws at the soul
While the emotional weight of managing side effects can feel overwhelming, it is important to remember that you are not alone in this journey. Engaging with a mental health professional, joining peer support groups, and maintaining a consistent routine can significantly alleviate the burden. Small, sustainable lifestyle adjustments often complement the pharmacologic therapy, enhancing overall well‑being.
yeah, i totally get u parth u dont have to feel so alone we can all chat and share tips its ok to ask doc bout dose tweaks keep it chill and dontstress
It is incumbent upon the discerning reader to recognize that the pharmaceutical narrative surrounding paroxetine is not merely a compilation of clinical data but a meticulously crafted tapestry of corporate interests, regulatory acquiescence, and covert lobbying. The disproportionate emphasis on efficacy over long‑term safety metrics, coupled with the suppression of independent studies that highlight cardiometabolic risks, suggests an orchestrated effort to maintain market dominance. Consequently, patients should critically evaluate the provenance of information and consider alternative therapeutics that have escaped such pervasive influence.