REMS Cost Calculator
Estimate implementation and ongoing compliance costs for different types of FDA Risk Evaluation and Mitigation Strategies (REMS) programs. The calculator uses industry-standard cost data to provide realistic estimates based on your program type.
Estimated Annual Costs
$0
- Implementation: $0
- Compliance & Maintenance: $0
- Training & Certification: $0
Note: Costs based on FDA-PhRMA data (2023). Actual implementation costs may vary based on program size, geography, and specific requirements. Simple programs cost $500k-$1M to implement; complex ETASU systems can exceed $15M annually.
Risk Evaluation and Mitigation Strategies (REMS) is a formal program created by the U.S. Food and Drug Administration (FDA) to manage drugs that carry serious safety risks. By attaching extra safeguards-like special training, patient registries, or medication guides-REMS aims to keep the benefits of a high‑risk medication higher than its dangers.
Why REMS Exists: The Core Problem
Imagine a life‑saving cancer pill that can also trigger deadly liver failure if taken without close monitoring. Traditional labeling would list the risk, but doctors and patients might miss the nuance. REMS forces a “extra layer” of oversight so that the most dangerous side effects get real‑time checks, lab tests, or controlled dispensing. The FDA launched this structure under the 2007 FDA Amendments Act, and it has grown from a handful of programs in 2007 to 78 active REMS covering roughly 150 medications by 2023.
Who Needs to Know About REMS?
- Prescribers - Must complete training, certify competence, and sometimes enroll patients in registries.
- Pharmacists - Verify patient eligibility, follow special dispensing rules, and document compliance.
- Patients - May receive medication guides, consent forms, and periodic lab‑test appointments.
- Drug Sponsors - Design, submit, and maintain the REMS program throughout a drug’s lifecycle.
- Regulators - The FDA monitors performance metrics and can modify or sunset a REMS when risks change.
Key Elements That Make Up a REMS
Every REMS is customized, but most contain a mix of the following components:
- Medication Guide - A concise, patient‑focused pamphlet that explains the most serious risks and what to do if they occur.
- Communication Plan - Targeted outreach to doctors, pharmacists, and sometimes the public, ensuring everyone knows the safety steps.
- Elements to Assure Safe Use (ETASU) - The heavy‑weight items: prescriber certification, patient enrollment, special pharmacy settings, or required lab monitoring.
Comparing the Three Main REMS Elements
| Element | Primary Audience | Typical Action Required | Examples |
|---|---|---|---|
| Medication Guide | Patients | Read and acknowledge receipt | Isotretinoin iPLEDGE guide, Thalidomide risk guide |
| Communication Plan | Prescribers & Pharmacists | Webinars, emailed bulletins, CME credits | Zyprexa Relprevv prescriber notice, opioid education outreach |
| ETASU | Prescribers, Pharmacies, Patients | Certification, registry enrollment, lab monitoring, restricted dispensing sites | Clozapine weekly ANC testing, iPLEDGE enrollment, long‑acting injectable monitoring |

Real‑World REMS in Action
Let’s walk through two well‑known programs to see how the pieces fit.
1️⃣ Isotretinoin (Accutane) - iPLEDGE
The drug can cause severe birth defects, so the FDA requires a three‑step REMS:
- Prescriber and pharmacy must be registered in the iPLEDGE system.
- Female patients of child‑bearing potential must complete monthly pregnancy tests and sign a consent.
- Pharmacies verify both prescriber and patient enrollment before dispensing.
Physicians report an average 3‑7‑day delay before the first fill, but the program has prevented thousands of fetal exposures.
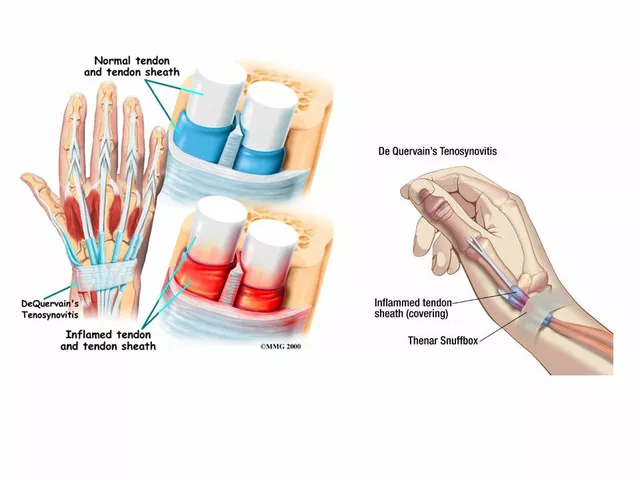
2️⃣ Clozapine - Blood‑Monitoring REMS
Clozapine can cause agranulocytosis, a potentially fatal drop in white blood cells. The REMS mandates:
- Weekly absolute neutrophil count (ANC) tests for the first 6 months, then bi‑weekly.
- Prescriber certification that they understand the monitoring schedule.
- Pharmacy verification of the latest lab results before each dispense.
Hospitals estimate an extra 15‑20 minutes per prescription, yet the monitoring has cut agranulocytosis cases by over 90% since implementation.
How REMS Differs From Other Safety Systems
In Europe, every new medicine must submit a Risk Management Plan (RMP), regardless of risk level. The U.S. reserves REMS for the ~5% of drugs with serious safety concerns. Unlike post‑marketing surveillance, which relies on voluntary adverse‑event reporting, REMS forces proactive actions before a drug reaches the patient.
Benefits and Criticisms: What the Data Says
Proponents argue that REMS makes it possible to approve high‑impact therapies that would otherwise be barred. A 2022 FDA round‑table quoted Dr. Robert Temple saying REMS “has been essential for bringing critical therapies to market.” On the flip side, a 2019 JAMA Internal Medicine analysis found REMS added an average of 5.4 days to first prescription, and a 2021 Harvard testimony highlighted unnecessary burdens for some opioid REMS programs.
Surveys of clinicians paint a mixed picture: 68% of physicians say REMS delays affect patient outcomes, while 73% of pharmacists cite extra administrative hours each week. The FDA’s own 2023 “REMS Integration Initiative” reduced platform fragmentation, consolidating 22 of 78 programs onto a single portal, but only 35% of programs now talk directly to electronic health records.
Cost of Compliance
The industry spends roughly $1.2 billion a year on REMS. Simple programs (just a medication guide) cost about $500,000 to develop; complex ETASU systems-think patient registries, weekly labs, and certified dispensing sites-can exceed $15 million annually. Non‑compliance isn’t cheap either: the FDA issued 17 warning letters in FY 2022, with the biggest settlement at $2.1 million for a clozapine REMS failure.
Future Directions: Digital Health and Sunset Strategies
Starting in 2024, the FDA’s strategic plan pushes REMS toward digital tools. Pilot apps now collect real‑time blood‑test data for anticoagulants, reducing the need for in‑person lab visits. The agency also began “sunsetting” REMS that are no longer justified-thalidomide’s program ended in 2023 after two decades of safe use and alternative risk controls.
Looking ahead, analysts predict 45% of new oncology drugs will carry a REMS by 2027, up from 38% in 2023. However, a 2023 FDA‑PhRMA task‑force report warned that 63% of existing REMS lack validated metrics to prove they truly improve safety without hurting access. The push for measurable outcomes is likely to shape the next wave of program redesigns.
Practical Checklist for Healthcare Professionals
- Verify whether a prescribed drug has an active REMS before writing the order.
- Complete any required prescriber training; most modules are 1‑2 hours and available online.
- Enroll patients in the appropriate registry (e.g., iPLEDGE, clozapine). Keep enrollment numbers handy.
- Schedule required labs and document results in the EHR; note the REMS‑specific window (weekly, bi‑weekly, etc.).
- Use the FDA’s centralized REMS portal to confirm dispensing eligibility; screen captures can serve as audit evidence.
- Monitor your institution’s compliance dashboards; aim for >90% on‑time completion rates to avoid penalties.
Key Takeaways
- REMS is a targeted FDA safety program for drugs with serious, manageable risks.
- Core elements include Medication Guides, Communication Plans, and ETASU.
- Implementation costs are high, but they enable access to life‑saving therapies.
- Clinicians face workflow challenges; digital tools and integration initiatives are reducing the burden.
- Future REMS will rely more on real‑time monitoring and clear metrics of benefit versus access barriers.
What types of drugs require a REMS?
FA D A typically applies REMS to drugs with serious safety concerns that can be mitigated through specific actions-examples include isotretinoin (birth‑defect risk), clozapine (agranulocytosis), and many oncology agents with severe immune‑system effects.
How do prescribers get certified for an ETASU REMS?
Certification is usually an online module approved by the FDA. It takes 1‑2 hours, covers the drug’s risk profile, required monitoring, and documentation steps. After passing a short quiz, the prescriber receives a digital badge that must be uploaded to the REMS portal.
Can a REMS be removed once a drug is proven safe?
Yes. The FDA can “sunset” a REMS when data show the additional safeguards no longer add value. Thalidomide’s REMS was discontinued in 2023 after two decades of safe use and alternative risk‑management tactics.
What impact does REMS have on patient access?
Studies show a modest delay-average 5‑6 days-to first prescription, especially for rare‑disease drugs. However, for high‑risk therapies the trade‑off is often worth it because severe adverse events are dramatically reduced.
How are digital health tools changing REMS?
Pilot apps now let patients upload lab results directly to the FDA’s REMS portal, cutting manual paperwork. Real‑time alerts can trigger a pharmacist to intervene before a dangerous dose is given, streamlining safety while keeping care convenient.


So, let’s just get this straight, the whole REMS circus isn’t some heroic guardian of patient safety, it’s more like a bureaucratic nightmare that keeps good meds from gettin’ to the folks who need ‘em.
First off, the FDA’s idea that you need a whole registry, a set of labs, and a certification just to write a prescription sounds like they’re trying to add extra layers to a problem that’s already complicated enough.
You’ve got prescribers spendin’ hours on modules that could’ve been a quick coffee‑chat, pharmacists juggling paperwork while the patient waits, and patients that end up missing doses because the red tape is slower than a snail on a sidewalk.
And don’t even get me started on the cost-billions of dollars a year, yet the data on actual lives saved is as thin as the paper the FDA prints its guidelines on.
Look, I get the whole “high‑risk meds need extra oversight” thing, but the way it’s implemented feels more like a power‑trip for regulators than a real safety net.
The iPLEDGE program, for instance, has reduced fetal exposures, sure, but it also creates a 5‑day delay that can be the difference between a tumor shrinking and it marching on.
Clozapine monitoring? Absolutely necessary, but the weekly ANC tests feel like a hammer for a nail when you could use more targeted biomarkers.
The whole point of these programs is to protect, but when you make the barriers so high that clinicians start finding loopholes, you’re just shifting the risk elsewhere.
And let’s be honest, there are plenty of drugs that slip through the cracks without a REMS, yet they don’t cause the apocalypse.
If the FDA truly cared about outcomes, they’d focus on smarter, data‑driven triggers instead of blanket requirements that treat every prescriber like a rookie.
The digital health pilot apps are a step in the right direction, but they’re still in the sandbox while the rest of the system is stuck in the stone age.
Bottom line: we need a balanced approach, not a one‑size‑fits‑all draconian checklist that punishes both patients and providers.
Meanwhile, the administrative burden drives some clinicians to avoid prescribing the most effective treatments altogether, which defeats the very purpose of these drugs.
In short, let’s re‑engineer REMS to be risk‑adaptive, not risk‑averse.
When evaluating the impact of REMS, it’s crucial to separate anecdotal inconvenience from measurable safety outcomes.
The recent FDA data shows a modest reduction in adverse events for high‑risk therapies, yet the statistical significance remains borderline.
Administrative time spent on certification could be reallocated to direct patient care, which would likely improve overall health metrics.
Furthermore, the variance in compliance across institutions suggests that a one‑size‑fits‑all model may be suboptimal.
Targeted risk‑based adjustments, supported by real‑world evidence, could streamline processes without compromising safety.
It is truly astonishing how the regulatory framework has managed to reinvent the wheel with such enthusiastic fervor.
One might posit that the sheer volume of paperwork associated with each REMS entry serves as an elegant reminder of the FDA’s unwavering commitment to bureaucracy.
In reality, however, the marginal gain in patient safety appears to be eclipsed by the cumulative burden imposed on prescribers and pharmacists alike.
Consider, for example, the iPLEDGE enrollment workflow, which obliges a seemingly endless chain of consents, lab orders, and electronic verifications before a single tablet can be dispensed.
While the intention is commendable, the execution borders on theatrical excess, transforming routine care into a performance art piece.
Moreover, the cost implications-both financial and temporal-are non‑trivial, especially for smaller practices that lack dedicated compliance staff.
It would be prudent for the agency to adopt a more nuanced, data‑driven approach, prioritizing interventions with demonstrable benefit over procedural vanity.
In short, let us not mistake the appearance of diligence for genuine progress.
Hey, I totally get the frustration, but there’s actually a silver lining hidden in all those extra steps.
When we see patients get the right monitoring, like those weekly ANC checks for clozapine, it’s a reminder that the system is watching out for them.
Sure, it feels like a slowdown, but think of it as a safety net that catches the rare but scary side‑effects before they become a nightmare.
And hey, with the new digital apps rolling out, those paperwork mountains might shrink faster than we expect.
So maybe it’s not all doom and gloom – there’s a chance the process will evolve into something smoother for everyone.
While the optimism expressed is appreciated, an objective assessment reveals that the incremental benefit derived from these monitoring protocols is statistically marginal.
The cost‑benefit analyses published in peer‑reviewed journals indicate that the majority of adverse events prevented could be addressed through more selective, risk‑based criteria.
Broad‑spectrum REMS requirements, as currently implemented, generate unnecessary administrative overhead, diverting resources from direct patient care.
A recalibration of the framework, predicated on robust predictive modeling, would likely yield superior outcomes with reduced systemic strain.
It is evident that REMS programs embody a complex balance between safeguarding public health and preserving clinical efficiency.
A collaborative approach, engaging regulators, clinicians, and patient advocacy groups, could foster more adaptable risk mitigation strategies.
By incorporating real‑world evidence and flexible monitoring tiers, the system may achieve enhanced safety without imposing undue burdens on healthcare providers.
Such dialogue‑driven reforms would honor both the imperative of patient protection and the practical realities of medical practice.
Listen, all that high‑falutin talk about “collaborative approaches” sounds nice on paper, but on the ground it’s just another excuse for endless meetings and paperwork.
If we keep sugar‑coating the fact that REMS are a massive hassle, we’ll never cut the red‑tape that chokes our clinics.
It’s time to smash the status quo and demand a streamlined, no‑nonsense system that gets drugs to patients without the bureaucratic circus.
Indeed, the current paradigm suffers from what could be termed “regulatory inertia syndrome,” wherein iterative policy refinements become self‑propagating feedback loops that amplify administrative latency.
From a systems‑engineering perspective, the lack of modular interoperability between the REMS portal and electronic health record platforms exacerbates the cognitive load on providers.
Adopting API‑first architectures and real‑time data pipelines could mitigate these friction points, effectively reducing the “process latency” metric.
Nevertheless, the cultural shift required to embrace such digital transformation remains a formidable barrier, demanding both stakeholder buy‑in and resource allocation.
We’re all in this together, keep learning.
Indeed, fostering a shared understanding among clinicians, regulators, and patients is essential to ensuring that safety protocols are both effective and sustainable.
What most people don’t realize is that REMS is less about protecting patients and more about giving the pharmaceutical lobby leverage over the FDA.
The timing of new REMS rollouts often coincides with major patent extensions, suggesting a coordinated effort to extend market exclusivity.
Insiders have hinted that the data used to justify these programs are selectively presented, masking the true cost‑benefit ratio.
Furthermore, the opaque nature of the decision‑making process means that external oversight is virtually nonexistent.
When you connect the dots – the increased fees, the mandatory training modules, the endless paperwork – you see a pattern of revenue generation rather than risk mitigation.
Even the recent push for digital health tools appears designed to harvest patient data for secondary markets, under the guise of compliance.
It’s no coincidence that the agencies funding these digital platforms are also the ones imposing the REMS obligations.
In short, the whole system feels engineered to keep the industry’s cash flow robust while pretending to safeguard health.
Transparency and independent audit trails would be the only viable antidotes to this self‑serving apparatus.
The argument presented, while evocative, overlooks the extensive empirical evidence supporting REMS efficacy in mitigating severe adverse events.
Rigorous post‑marketing surveillance data demonstrate a statistically significant reduction in incidence rates for high‑risk pharmacotherapies under the REMS framework.
Consequently, any critique should be grounded in comprehensive quantitative analysis rather than conjectural associations.
It remains incumbent upon policymakers to balance vigilance with pragmatism, ensuring that patient safety remains paramount.