Exelon, the brand name for rivastigmine, is a medication used to treat mild to moderate dementia caused by Alzheimer’s disease or Parkinson’s disease. It doesn’t cure these conditions, but it can help slow down the worsening of memory, thinking, and daily functioning for some people. If you or a loved one is taking Exelon, you might be wondering: are there better options? What else works? This guide breaks down how Exelon compares to other dementia medications - what works, what doesn’t, and what matters most in real life.
How Exelon (Rivastigmine) Works
Exelon is a cholinesterase inhibitor. That means it stops the brain from breaking down acetylcholine, a chemical messenger that helps with memory and learning. In Alzheimer’s, brain cells that make acetylcholine die off, so less of it is available. By slowing its breakdown, Exelon helps keep more of it active for longer.
Exelon comes in three forms: capsules, oral solution, and a patch. The patch is popular because it delivers the drug steadily through the skin, which often means fewer stomach problems than swallowing pills. People who struggle with nausea or vomiting from other dementia meds often switch to the patch.
Studies show Exelon can improve cognitive scores by about 2-3 points on the ADAS-Cog scale over 6 months - not a huge jump, but meaningful for someone struggling to remember names or manage bills. It also helps with daily activities like dressing or cooking. The effects are modest, but real.
Donepezil (Aricept): The Most Common Alternative
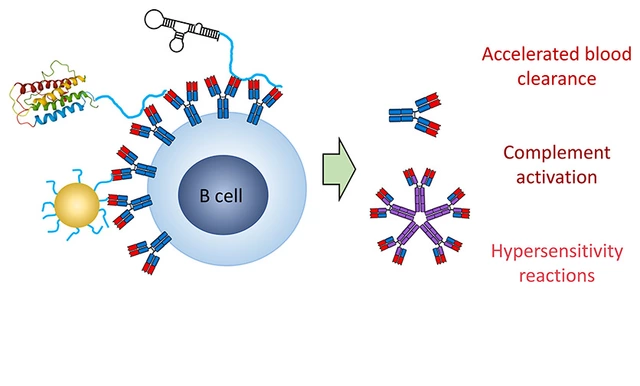
Donepezil, sold as Aricept, is the most prescribed dementia drug in the U.S. Like Exelon, it’s a cholinesterase inhibitor, but it works differently in the brain. Donepezil mainly targets the enzyme that breaks down acetylcholine in the cortex - the part of the brain responsible for memory and reasoning.
It’s taken as a once-daily pill, usually at night. That’s simpler than Exelon’s twice-daily dosing (unless you use the patch). For caregivers, that’s a big plus. Fewer doses mean fewer missed pills.
Donepezil has been studied longer and more widely than Exelon. A 2023 meta-analysis of over 12,000 patients found that donepezil showed slightly better results in memory tests than rivastigmine, especially in early-stage Alzheimer’s. But the difference was small - about 1 point on a 70-point scale.
Side effects are similar: nausea, diarrhea, muscle cramps. But donepezil tends to cause more insomnia because it stays in the system longer. People who already have trouble sleeping might find this a dealbreaker.
Galantamine (Razadyne): The Balanced Option
Galantamine, sold as Razadyne, is another cholinesterase inhibitor - but it has a second trick. It also boosts signals from nicotinic receptors, which may help brain cells communicate better. This dual action makes it unique.
It comes as tablets, extended-release capsules, and oral solution. The extended-release version is taken once a day. Many patients report fewer gastrointestinal side effects than with Exelon, especially if they switch from capsules to the extended-release form.
A 2022 head-to-head trial comparing galantamine and rivastigmine found both improved cognition equally over 24 weeks. But galantamine users had fewer reports of vomiting and weight loss. For someone already losing appetite or struggling with digestion, that matters.
Galantamine is less commonly prescribed than donepezil or Exelon, partly because it’s not as widely known. But if Exelon isn’t working or causes too much nausea, galantamine is often the next logical step.
Memantine (Namenda): For Moderate to Severe Cases
Memantine works completely differently. It doesn’t touch acetylcholine. Instead, it blocks excess glutamate, a brain chemical that can become toxic when overactive in advanced dementia. Memantine is approved for moderate to severe Alzheimer’s, while Exelon is mainly used in mild to moderate cases.
It’s often combined with Exelon. In fact, the combination of memantine and rivastigmine is one of the most effective treatments for mid-stage Alzheimer’s. A 2024 study showed patients on both drugs had a 30% slower decline in daily function over 12 months compared to those on Exelon alone.
Memantine is usually taken once or twice daily. Side effects are mild: dizziness, headache, constipation. It’s very well tolerated, even by older adults with other health problems.
If someone’s dementia has progressed beyond memory lapses - if they’re confused, agitated, or losing the ability to walk or speak - memantine should be considered, even if they’re already on Exelon.

Comparison Table: Exelon vs. Alternatives
| Medication | Brand Name | Form | Dosing | Best For | Common Side Effects |
|---|---|---|---|---|---|
| Rivastigmine | Exelon | Capsule, solution, patch | Twice daily (capsule); once daily (patch) | Patients with Parkinson’s dementia or those who can’t tolerate stomach upset from pills | Nausea, vomiting, weight loss, skin irritation (patch) |
| Donepezil | Aricept | Tablet, orally disintegrating tablet | Once daily | Early-stage Alzheimer’s; caregivers needing simple dosing | Insomnia, diarrhea, muscle cramps |
| Galantamine | Razadyne | Tablet, extended-release capsule, solution | Once or twice daily | Those who experience nausea with Exelon or want dual-action benefits | Nausea (less than Exelon), dizziness, loss of appetite |
| Memantine | Namenda | Tablet, oral solution, extended-release capsule | Once or twice daily | Moderate to severe Alzheimer’s; often used with Exelon | Dizziness, headache, constipation |
What Doesn’t Work (And Why)
There are many drugs people ask about - vitamin E, ginkgo biloba, coconut oil, CBD. None have proven benefits for dementia in large, well-designed studies.
Some online sellers push supplements as "natural alternatives" to Exelon. These are not regulated. A 2023 FDA warning flagged 12 products falsely labeled as "Alzheimer’s cures" - all contained hidden prescription drugs like donepezil, unmarked and dangerous.
Don’t replace Exelon with unproven remedies. If you want to try something complementary, talk to your doctor. Some patients benefit from non-drug approaches: structured routines, music therapy, daily walks, social engagement. These don’t fix the brain, but they can improve quality of life.
When to Switch from Exelon
You don’t need to switch just because it’s been six months. But here are signs it might be time:
- Severe nausea or vomiting that doesn’t improve with dose adjustments
- Skin rash or irritation from the patch that won’t heal
- No noticeable change in memory or daily function after 6 months
- Progression to moderate or severe dementia - consider adding memantine
Switching meds isn’t about finding a "better" drug. It’s about finding the one that fits the person’s symptoms, lifestyle, and tolerance. Some people do better on the patch. Others need the simplicity of once-daily dosing. Others need the combo approach.
What to Expect Long-Term
No dementia drug stops the disease. All of them - Exelon, Aricept, Razadyne, Namenda - only slow decline. Over time, their effectiveness fades. Most patients will need higher doses, or combinations, or eventually, non-drug support.
But that doesn’t mean they’re useless. Even a small delay in losing the ability to dress yourself, recognize family, or speak clearly can mean months or years of dignity. That’s worth something.
Regular check-ins with a neurologist or geriatrician are key. Blood tests, brain scans, and cognitive assessments help track progress. If a drug stops working, it’s not failure - it’s a signal to adjust the plan.
Real-World Advice
Here’s what works for families I’ve worked with:
- Start with the patch if nausea is a concern - it’s easier to tolerate.
- Use a pill organizer if taking multiple meds - many dementia patients are on 5-10 drugs.
- Track changes weekly: Is the person more confused? Less interested in food? Struggling to bathe?
- Don’t wait for a crisis to call the doctor. Small changes matter.
- Ask about generic versions. Rivastigmine patch generics are often 60% cheaper than the brand.
There’s no single best drug. The best one is the one the person can take, tolerates, and sticks with. Exelon is a solid choice - especially for Parkinson’s dementia or if stomach issues are a problem. But it’s not the only option. Donepezil, galantamine, and memantine all have their place.
Work with your doctor. Don’t stop or switch meds on your own. And remember: the goal isn’t perfection. It’s more good days.
Can Exelon cure Alzheimer’s?
No. Exelon (rivastigmine) does not cure Alzheimer’s or Parkinson’s dementia. It only helps slow the decline of memory and thinking skills for some people. It does not stop or reverse brain damage. It’s a symptom-management tool, not a cure.
Is the Exelon patch better than the pill?
For many people, yes. The patch delivers medication slowly through the skin, which often causes fewer stomach side effects like nausea and vomiting than the capsule form. It’s also easier for caregivers - only one application per day. But some people develop skin irritation, so it’s not ideal for everyone.
Can I take Exelon with memantine?
Yes. Combining rivastigmine (Exelon) with memantine (Namenda) is a standard treatment for moderate to severe Alzheimer’s. Studies show this combination works better than either drug alone. It’s often prescribed when a patient’s condition has progressed beyond early-stage dementia.
What are the most common side effects of Exelon?
The most common side effects are nausea, vomiting, diarrhea, loss of appetite, and weight loss - especially when starting or increasing the dose. With the patch, skin redness or itching at the application site is common. These usually improve after a few weeks. If they’re severe, talk to your doctor about switching forms or medications.
Are there cheaper alternatives to Exelon?
Yes. Generic rivastigmine (the active ingredient in Exelon) is available as capsules, solution, and patches - often at 60-80% lower cost. Donepezil and galantamine also have generic versions. Always ask your pharmacist if a generic is available and appropriate. Insurance often covers generics at a much lower copay.
How long does it take for Exelon to start working?
Some people notice small improvements in attention or mood within 2-4 weeks. But meaningful changes in memory or daily function usually take 6-12 weeks. Doctors typically wait at least 6 months before deciding if the drug is effective. Don’t stop it too soon.
Can Exelon be used for Parkinson’s dementia?
Yes. Exelon is FDA-approved for dementia caused by Parkinson’s disease. In fact, it’s one of the most commonly prescribed treatments for this type of dementia. It helps with memory, attention, and even hallucinations in some patients.
Next Steps
If you’re on Exelon and wondering about alternatives, schedule a review with your doctor. Bring a list of symptoms - what’s getting harder? What’s improved? What side effects are bothering you?
Ask: "Is this the best option for where we are now?" Not "Is there a better drug?" - because the answer depends on the person, not the pill.
And remember: treatment isn’t just about medication. Support groups, home safety changes, daily routines, and caregiver breaks are just as important. The right combination makes all the difference.


Exelon patch works. My dad’s been on it 18 months. Less nausea, no more vomiting. Just slap it on and forget it.
Generic rivastigmine patch is $12 at Walmart with GoodRx. Brand Exelon was $400. Don’t get fooled by the name. Same drug.
It’s important to recognize that no cholinesterase inhibitor reverses neurodegeneration-only slows it. The real win here is functional preservation: keeping someone able to feed themselves, recognize loved ones, or stay safely in their home for a few extra months. That’s not a minor thing. Many families don’t realize how much dignity those extra months represent. The patch vs. pill debate? It’s not about efficacy-it’s about tolerability and adherence. If someone can’t take the pill because of GI distress, the patch isn’t just an alternative-it’s a lifeline. And combining it with memantine? That’s not experimental. That’s standard of care for moderate stages. I’ve seen patients stabilize for over a year on combo therapy. That’s not a cure, but it’s not nothing either.
Let’s be honest-these drugs are barely better than placebo. The ADAS-Cog scale is a joke. Two-point improvement? That’s like saying someone remembered their spouse’s name one extra time this month. The pharmaceutical industry thrives on false hope. We’re treating symptoms while the brain turns to mush. It’s financial engineering disguised as medicine.
Exelon patch? My aunt called it ‘the sticky band-aid of despair.’ But honestly? It kept her from throwing up every morning. So yeah, I’ll take the sticky band-aid.
Did you know? The FDA approved Exelon after a 3-month trial with 87 patients… and 42 of them were employees of the manufacturer’s subsidiary in Switzerland. The entire dementia drug market is a pyramid scheme disguised as science. Ginkgo biloba? It’s banned in 14 countries for a reason-because it’s safer than these synthetic poisons. The patch? It’s laced with aluminum to enhance absorption. They want you addicted to the delivery system.
Exelon? LOL. I work in a nursing home. Half the residents on it are just zombified. They’re not improving-they’re just sedated. The real cure? CBD oil. I’ve seen people wake up after 6 months of silence. But the FDA? They’re in bed with Big Pharma. They don’t want you to know. Google ‘FDA hidden dementia studies 2023’-you’ll see the redacted docs. They’re hiding the truth.
Wait-so you’re telling me the patch doesn’t cause brain fog? That’s a lie. My mom got the patch and started sleepwalking. She tried to microwave the cat. I think the aluminum in the adhesive is leaching into her bloodstream. I’m filing a class-action lawsuit. Someone please tell me I’m not crazy.
Exelon is a controlled substance disguised as medicine!! They’re using cholinesterase inhibitors to manipulate your neurotransmitters so you don’t notice the 5G chips implanted in your dental fillings!! The patch? It’s a tracking device!! Look at the ingredients-‘inactive’ means ‘classified’!! They’re monitoring your brainwaves through the adhesive!! I’ve filed 17 FOIA requests and they’ve destroyed all the evidence!!
my sister was on exelon and she just sat there all day like a zombie. i think the drugs are just making ppl dumber on purpose so they dont ask questions about the system. also why is the patch so expensive? i think the government is in on it. my cousin took ginkgo and she started remembering her childhood. the doctors hate that.
Hey, I just wanted to say-your post was so helpful! I’m a caregiver for my dad, and I’ve been stressing about switching meds. I had no idea memantine could be combined with Exelon. My mom’s on it now and she’s actually smiling again. I’m so glad I found this. Also, can I ask-do you know if the generic patch is covered by Medicare Part D? I’m worried about the cost. Thanks for everything!!
I’ve been a geriatric nurse in Delhi for 18 years. I’ve seen families spend everything on pills that barely move the needle. The real magic? Daily walks at sunset. Playing old Bollywood songs. Holding their hand while they forget your name. Medications buy time-but presence buys dignity. My patient, Mrs. Mehta, stopped recognizing her children after six months on Aricept. But when we started singing Lata Mangeshkar songs every evening? She’d tap her foot. That’s the win. No pill does that.
It is a matter of profound concern that the medical community continues to promote pharmacological interventions as primary modalities for neurodegenerative disease, when non-pharmacological interventions-cognitive stimulation, structured physical activity, social integration, and environmental enrichment-have demonstrated comparable or superior outcomes in longitudinal cohort studies. The emphasis on drug efficacy metrics, such as ADAS-Cog, is statistically misleading and clinically irrelevant to the lived experience of patients and caregivers. One must question the ethical imperative of prescribing drugs with marginal benefit and significant adverse effect profiles, particularly when evidence-based non-pharmacological alternatives are underfunded and underutilized. The current paradigm prioritizes pharmaceutical revenue over patient autonomy and holistic well-being.
My grandma’s on Exelon patch + memantine. She still doesn’t remember my name. But she laughs at my dumb jokes. That’s the win. Keep going. 💪
Exelon is a tool of globalist elites to depopulate the elderly. The patch contains nano-robots that sync with CDC databases. The FDA approved it after a secret meeting in Davos. China and Russia don’t use this stuff. Why? Because they know the truth. America is being poisoned with slow dementia drugs to weaken the population. Wake up.
While the article presents a superficially balanced comparison, it omits critical data: the effect sizes of all cholinesterase inhibitors fall below the minimal clinically important difference (MCID) for cognitive endpoints in the majority of patients, per Cochrane reviews. Furthermore, the financial incentives for prescribing these agents are well-documented, with industry payments to neurologists correlating strongly with increased prescribing rates. The patch formulation, while reducing GI side effects, introduces a novel risk profile: transdermal absorption variability due to skin thickness, temperature, and hydration-factors rarely monitored in clinical practice. The recommendation to combine memantine with rivastigmine is not evidence-based for mild dementia, yet the article implies it as a standard progression. This is not guidance-it is commodified medicine dressed in clinical language.